Differences in tissue-specific utilization of NAD+ boosters (NAD+ flux study) | Rhonda Patrick
Get the full length version of this episode as a podcast.
This episode will make a great companion for a long drive.
The Omega-3 Supplementation Guide
A blueprint for choosing the right fish oil supplement — filled with specific recommendations, guidelines for interpreting testing data, and dosage protocols.
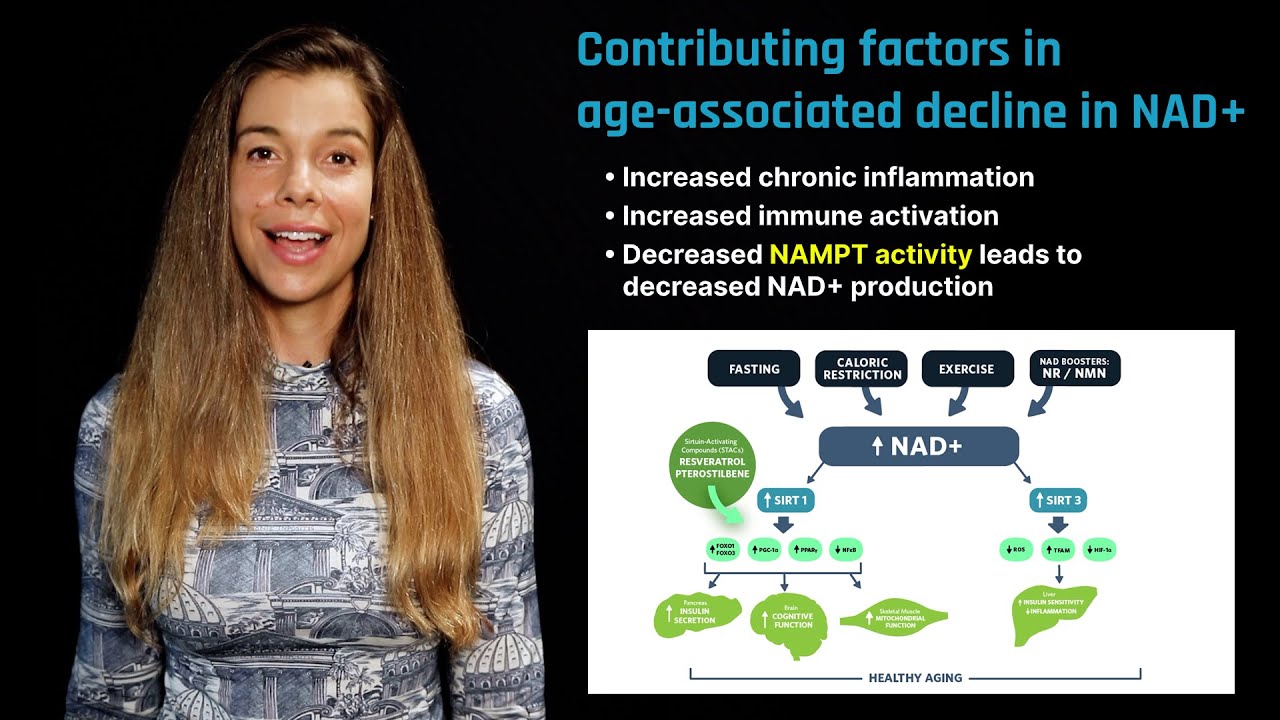
In 2018 Liu et al. investigated the metabolic fate and distribution of varying doses of nicotinamide riboside (NR) and nicotinamide mononucleotide (NMN) administered either by oral gavage or intravenously to animals. What the study found was that when NR or NMN was orally administered to animals, NAD+ levels increased in a dose-dependent manner in the liver, kidney, muscle, and brain. However, all of the orally administered NR and NMN was converted to nicotinamide in the liver, so the NAD+ found in other tissues was derived from the salvage pathway and not directly from NR or NMN.
When administered intravenously, NR and NMN did reach the liver, kidney, and muscle tissues, raising NAD+ levels in a dose-dependent manner. In some tissues, NR did so somewhat more successfully. However, neither NR nor NMN crossed the blood-brain barrier. Brain levels of NAD+ did increase indirectly by way of NAD+ derived from the salvage pathway, which requires conversion to nicotinamide as an intermediary step.
The question of whether NAD+ is derived directly from NR or NMN in certain tissues rather than being salvaged from nicotinamide may, in particular, have implications for whether or not oral administration may be hampered in achieving maximal NAD+ status due to the fact that the process of salvaging NAD+ from nicotinamide is subject to feedback inhibition.
For this reason, the fact that intravenous administration of NMN or NR (particularly NR) is more successful suggests that oral administration may have certain limitations that intravenous does not. However, more human research is needed, possibly with higher doses. Furthermore, it is notable that improved NAD+ status happened in virtually all tissues tested at all doses (oral and intravenous), despite the often predominant involvement of the salvage pathway.
Rhonda: The next point of concern is the bioavailability of either nicotinamide riboside or nicotinamide mononucleotide. The important point to address is whether nicotinamide riboside or nicotinamide mononucleotide can reach other tissues intact and directly form NAD+ without going through that NAD+ recycling pathway that I mentioned earlier called the salvage pathway. The salvage pathway would mean that nicotinamide riboside or nicotinamide mononucleotide were first metabolized into just nicotinamide before forming NAD+ instead of directly forming NAD+. This is an important point because NAD+ produced from the salvage pathway is subject to feedback inhibition, and therefore, cannot raise NAD+ levels in tissues above a certain level.
So, let's talk about some details. An animal study using isotope tracers allowed NAD+ made directly from nicotinamide riboside or directly from nicotinamide mononucleotide versus NAD+ made from nicotinamide via the salvage pathway to be measured. What the study found was that at a low oral dose of around 50 milligrams per kilogram body weight of either nicotinamide riboside or nicotinamide mononucleotide, they produced very low levels of NAD+ made directly from those precursors, but only in the liver, not in other tissues. Low levels of nicotinamide-derived NAD+, on the other hand, were found in the kidneys and very low levels of nicotinamide-derived NAD+ were found in the muscles and also in the brain. The human equivalent dose of 50 milligrams per kilogram body weight is roughly 4.07 milligrams per kilogram body weight. So, for a 180-pound person, that is approximately 332 milligrams of either nicotinamide riboside or nicotinamide mononucleotide, which is a pretty doable dose, but very little increases in NAD+ were found, at least in animals at that dose.
A higher oral dose was also done, but only for nicotinamide riboside. A dose of 200 milligrams per kilogram body weight of nicotinamide riboside showed no difference compared to a low dose in terms of making NAD+ direct from nicotinamide riboside in any other tissues other than the liver. However, more of the NAD+ derived from the salvage pathway was found in the kidney, muscle, and the brain than at the lower dose. So, 200 milligrams per kilogram body weight translates to around a human equivalent dose of 16.3 milligrams per kilogram body weight, which, for a 180-pound person, is about 1.3 grams, which is pretty high. When nicotinamide riboside or nicotinamide mononucleotide were given intravenously at varying doses, so 50 milligrams per kilogram body weight or 500 milligrams per kilogram body weight, directly produced NAD+ was found in the liver, kidney, and muscle in a dose-dependent manner.
However, the only NAD+ detected in the brain was that which was salvaged from nicotinamide, suggesting that neither nicotinamide riboside nor nicotinamide mononucleotide cross the blood-brain barrier. It is noteworthy that head-to-head comparison of identical doses of injected nicotinamide riboside and nicotinamide mononucleotide produced more NAD+ made directly from nicotinamide riboside in the liver, kidney, and, particularly, in the muscle tissue compared to nicotinamide mononucleotide. So, what does this all mean, and should we care? What this data from the isotope tracer studies means is that, even at very high oral doses, neither nicotinamide riboside or nicotinamide mononucleotide appeared to directly be transported to other tissues other than the liver, at least, again, at those doses that were measured. However, nicotinamide riboside and nicotinamide mononucleotide were converted into nicotinamide, which was then transported to other tissues, and some of that nicotinamide was then converted into NAD+. And, at the end of the day, isn't raising cellular NAD+ levels what is most important, anyway?
The other animal studies I previously mentioned that showed positive health benefits in tissues like the muscle or the brain were at a very high oral dose of nicotinamide riboside and nicotinamide mononucleotide. In fact, in some cases, they were double the dose. So, they were about 400 milligrams per kilogram body weight. So, it's possible that nicotinamide riboside and nicotinamide mononucleotide can be transported to other tissues other than the liver at very, very high oral doses, but that's yet to be shown. However, it's also possible that at very, very high doses, the NAD+ derived from the salvage pathway was high enough to do something beneficial.
The isotope data also suggests that if nicotinamide riboside or nicotinamide mononucleotide is administered intravenously, both of those compounds are able to be transported to other tissues and directly form NAD+ and not be subject to feedback inhibition. This also raises NAD+ levels in multiple tissues to a much higher concentration than otherwise would be. Of course, IV injection of these NAD+ boosters is very challenging to translate to humans. You may be wondering, why all the messing around with NAD+ boosters like nicotinamide riboside and nicotinamide mononucleotide in the first place? The reason nicotinamide riboside and nicotinamide mononucleotide are popular is because they can be transported into multiple tissue types, including the liver, kidney, muscle, and heart. The brain is the exception. Neither nicotinamide riboside nor nicotinamide mononucleotide seem to be able to directly cross the blood-brain barrier. But both form nicotinamide, which can be transported into all tissue types, including the brain, where it can then form NAD+. So, why not just go to the source and take or inject NAD+ directly? Well, for starters, NAD+ has poor bioavailability. Animal studies have shown that upon ingestion, orally administered NAD+ is primarily digested into the precursor, nicotinamide, but also to nicotinamide riboside and nicotinamide mononucleotide before being absorbed. While oral bioavailability of NAD+ is low, the hope is that intravenous NAD+ infusion may bypass the digestive system. The problem is that no mammalian NAD+ transporter has been identified. And with the exception of the brain and the heart, extracellular NAD+ has not been shown to be taken up into tissues.
When NAD+ was injected into the abdominal region of mice, it was able to raise NAD+ levels in some brain regions. Similarly, mice that were injected with a high dose of NAD+ had increased levels of NAD+ in the heart and also protection from cardiac hypertrophy. This suggests that direct injection of NAD+ at a high dose may be doing something beneficial, at least in the brain and in the heart. I would like to mention that just because no data exists, that does not mean that NAD+ delivered intravenously cannot raise NAD+ levels in other tissues other than the brain or the heart. It's possible that extracellular NAD+ could be metabolized to nicotinamide, and that could be transported to other tissues like the muscle, and also could be converted into NAD+. While there is very little preclinical data and zero clinical data on direct IV injection of NAD+, it does seem like this may also be a good idea or a good area to explore as a potential way to boost NAD+ levels in tissues.
The extent and rate at which drugs or other substances, such as plant-based dietary compounds, enter the body’s circulation. Bioavailability is influenced by a variety of factors, including dose, the presence of other foods or substances, and interindividual differences in metabolism due to gut absorptive surface and commensal microbial populations.
A highly selective semi-permeable barrier in the brain made up of endothelial cells connected by tight junctions. The blood-brain barrier separates the circulating blood from the brain's extracellular fluid in the central nervous system. Whereas water, lipid-soluble molecules, and some gases can pass through the blood-brain barrier via passive diffusion, molecules such as glucose and amino acids that are crucial to neural function enter via selective transport. The barrier prevents the entry of lipophilic substances that may be neurotoxic via an active transport mechanism.
Dietary supplements that purportedly increase cellular levels of nicotinamide adenine dinucleotide (NAD+). Examples of potential NAD+ boosters include resveratrol (a plant-based dietary compound found in grapes), metformin (a type of diabetes medication), and nicotinamide mononucleotide (a derivative of niacin).
Nicotinamide adenine dinucleotide (NAD) is a coenzyme found in all living cells used to transfer chemical energy from a food source to the electron transport chain. It exists in two forms, an oxidized and reduced form abbreviated as NAD+ and NADH respectively. NAD levels rise during a fasting state and activates the SIRT1 pathway. NADH levels rise during the fed state and serve as reducing equivalents to produce ATP.
A coenzyme that is required for the production of energy in cells. NAD+ is synthesized from three major precursors: tryptophan, nicotinic acid (vitamin B3), and nicotinamide. It regulates the activity of several key enzymes including those involved in metabolism and repairing DNA damage. NAD+ levels rise during a fasted state. A group of enzymes called sirtuins, which are a type of histone deacetylase, use NAD+ to remove acetyl groups from proteins and are important mediators for the effects of fasting, caloric restriction, and the effects of the plant compound resveratrol, a so-called caloric restriction mimetic.
A precursor molecule for the biosynthesis of nicotinamide adenine dinucleotide (NAD+), a coenzyme that participates in the production of cellular energy and repair. NMN helps maintain cellular levels of NAD+, thereby facilitating NAD+-dependent cellular activities, such as mitochondrial metabolism, regulation of sirtuins, and PARP activity. Animal studies have demonstrated that NMN administration is effective in increasing NAD+ levels across multiple tissues while improving the outcome of a variety of age-related diseases. Although NMN administration has proven to be safe and to effectively increase NAD+ levels in rodents, the safety and efficacy of NMN supplementation in humans remain unknown. NMN is available in supplement form and is present in various types of food, including broccoli, avocado, and beef. It is also an intermediate compound in the NAD+ salvage pathway, the recycling of nicotinamide into NAD+.
A precursor molecule for the biosynthesis of nicotinamide adenine dinucleotide (NAD+), a coenzyme that participates in the production of cellular energy and repair. NMN helps maintain cellular levels of NAD+, thereby facilitating NAD+-dependent cellular activities, such as mitochondrial metabolism, regulation of sirtuins, and PARP activity. Animal studies have demonstrated that NMN administration is effective in increasing NAD+ levels across multiple tissues while improving the outcome of a variety of age-related diseases. Although NMN administration has proven to be safe and to effectively increase NAD+ levels in rodents, the safety and efficacy of NMN supplementation in humans remain unknown. NMN is available in supplement form and is present in various types of food, including broccoli, avocado, and beef. It is also an intermediate compound in the NAD+ salvage pathway, the recycling of nicotinamide into NAD+.
One of four nitrogen-containing molecules that comprise DNA. A nucleotide consists of one of four chemicals, called a “base,” plus one molecule of sugar and one molecule of phosphoric acid. Nucleotides are typically identified by the first letter of their base names: adenine (A), cytosine (C), guanine (G), and thymine (T). They form specific pairs (A with T, and G with C), and their bonds provide the helical structure of the DNA strand.
Member only extras:
Learn more about the advantages of a premium membership by clicking below.
Get email updates with the latest curated healthspan research
Support our work

Every other week premium members receive a special edition newsletter that summarizes all of the latest healthspan research.
Comments
Aging News
- Vitamin D increases muscle strength and mass without altering body weight in mice.
- Any Level of Physical Activity Tied to Better Later-Life Memory
- Allulose Attenuated Age-Associated Sarcopenia via Regulating IGF-1 and Myostatin in Aged Mice
- Exercise increases activity of anti-aging sirtuin enzymes in older adults with obesity.
- Blood levels of sirtuin enzymes decline with Alzheimer's disease progression, making them a potential biomarker.