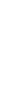


By becoming a member of FoundMyFitness premium, you'll receive the Science Digest every-other-week covering the latest in my exploration of recent science and the emerging story of better living — through deeper understandings of biology.
- Ketogenic diet, by replacing glucose with ketones as an energy source, lessens alcohol cravings among people with alcohol use disorders.
- Omega-3 fatty acids reduce the risk of cardiovascular disease-related death by up to 23 percent, especially in people with high triglyceride levels.
- Women see a 24 percent drop in premature death risk with just 140 minutes of weekly activity – half the time men need for similar benefits.
- Aging undermines the brain's capacity for maintaining working memory, with subtle declines in neuron activity and connectivity in the prefrontal cortex.
Sunburns are a major contributor to skin cancer risk, yet many people continue to get sunburned, with some experiencing multiple episodes each year. A recent study found that more than 30% of adults reported between one and five sunburns in the past year, and alcohol consumption was linked to an increased risk, with 21% of people who got sunburned having consumed alcohol at the time.
Researchers analyzed data from the 2022 Health Information National Trends Survey, which included more than 6,200 participants. They used statistical analysis to identify associations between sociodemographic factors, cancer risk perceptions, sun exposure behaviors, and the number of sunburns reported in the previous 12 months.
They found that 2.1% of participants reported more than six sunburns, 30.3% had between one and five, and 67.6% experienced none. Alcohol consumption was a contributing factor, with 21.5% of those who reported a sunburn also having consumed alcohol. Younger adults (aged 18 to 39) were more likely to experience sunburns than older adults, and men were at higher risk than women. Additionally, higher-income participants were more likely to get sunburned, with people in the highest income bracket more than four times as likely to report at least one sunburn in the past year.
These findings suggest that public health interventions should focus on groups most at risk for sunburns, including younger adults, men, and higher-income people. Addressing alcohol consumption during sun exposure could also help reduce sunburn incidence. Sunscreens can protect against sunburns, but some carry health risks. Learn more in this Q&A featuring Dr. Rhonda Patrick.
Tendons are essential for force transmission between muscles and bones. However, as people age, tendons lose collagen and stiffen, impairing athletic performance and increasing injury risk. A recent study found that combining resistance exercise with collagen supplementation enhanced tendon health in middle-aged men.
Researchers investigated the effects of 12 weeks of resistance exercise and collagen supplementation on patellar tendon properties in 20 middle-aged men. Both groups engaged in progressive lower-body resistance training twice weekly and received either 30 grams of hydrolyzed collagen or a placebo after training. The researchers evaluated the participants' tendon size, stiffness, and strength before and after the intervention.
They found that participants who took collagen experienced a greater increase in patellar tendon cross-sectional area (+6.8 mm²) than the placebo group (+1.2 mm²). They also experienced a twofold greater increase in tendon stiffness and measures of tendon strength than the placebo group. Both groups experienced muscle strength and explosive power improvements, but tendon adaptations were more pronounced with collagen supplementation.
These findings suggest that 12 weeks of resistance training with collagen supplementation enhances patellar tendon properties in middle-aged men. The patellar tendon is a strong, fibrous connective tissue that connects the bottom of the kneecap (patella) to the top of the shinbone (tibia). It plays a crucial role in movements like walking, running, jumping, and squatting, as it helps control the movement and stability of the knee joint. Learn more about the benefits of collagen supplementation in our overview article.
Microplastics may be more than environmental pollutants—they could contribute to the rise of drug-resistant bacteria. These tiny plastic fragments persist in wastewater, providing surfaces where bacteria congregate, form biofilms, and exchange genetic material that enhances antibiotic resistance. A recent study found that Escherichia coli cultured on microplastics were 171 times more resistant to the antibiotic ciprofloxacin than those grown on glass.
Researchers exposed E. coli to different types of microplastics—polyethylene, polystyrene, and polypropylene—at varying concentrations and sizes. They measured the bacteria’s survival rates and assessed whether they developed resistance to four common antibiotics: ampicillin, ciprofloxacin, doxycycline, and streptomycin. They also compared bacterial behavior on microplastics versus glass to determine how different surfaces influenced biofilm formation.
Bacteria attached to microplastics formed stronger biofilms and exhibited higher antibiotic resistance than those grown on glass. The water-repellant nature of the plastics, combined with their ability to attract and retain other substances, likely contributed to this effect. Bacteria grown in the presence of antibiotics and microplastics showed considerably greater resistance, with those exposed to ciprofloxacin displaying up to 171 times greater resistance and other antibiotics showing increases of up to 75 times.
These findings suggest that microplastics serve as breeding grounds for antibiotic resistance, potentially increasing the risk of persistent infections in environmental and healthcare settings. Addressing microplastic pollution may be crucial in slowing the spread of drug-resistant bacteria. Learn how to limit your exposure to microplastics in this episode featuring Dr. Rhonda Patrick.