#45 Dr. Matthew Walker on Sleep for Enhancing Learning, Creativity, Immunity, and Glymphatic System
This episode is available in a convenient podcast format.
These episodes make great companion listening for a long drive.
The Omega-3 Supplementation Guide
A blueprint for choosing the right fish oil supplement — filled with specific recommendations, guidelines for interpreting testing data, and dosage protocols.
Matthew Walker, Ph.D., is a professor of neuroscience and psychology at the University of California, Berkeley, and serves as the Director of the Center for Human Sleep Science. Formerly, Dr. Walker served as a professor of psychiatry at the Harvard Medical School.
Walker's research examines the impact of sleep on human health and disease. One area of interest focuses on identifying "vulnerability windows" during a person's life that make them more susceptible to amyloid-beta deposition from loss of slow wave sleep and, subsequently, Alzheimer's disease later in life.
Dr. Walker earned his undergraduate degree in neuroscience from the University of Nottingham, UK, and his Ph.D. in neurophysiology from the Medical Research Council, London, UK. He is the author of the New York Times best-selling book Why We Sleep: Unlocking the Power of Sleep and Dreams.
Sleep as foundational bedrock for our ability to learn from experience
"You can't pull the all-nighter and hope to be able to continue to learn." - Matthew Walker, Ph.D. Click To Tweet
In some ways, the highly conserved nature of sleep across the animal kingdom seems like a paradox: Whereas closing our eyes to sleep obviously leaves us and the rest of the animal kingdom vulnerable for long stretches of the twenty-four-hour day, not sleeping must carry even more risk when we consider that it has not been weeded out in spite of this.
Without sufficient sleep, our ability to learn – the acquisition of new memories – begins to rapidly break down. And yet, this is only one of the major roles we now appreciate that sleep has. In this episode, sleep expert Dr. Matt Walker describes how sleep is critical to learning and survival because it facilitates a process he likens to the input, storage, and transfer of data in a computer.
Sleep preps the brain for information input
The formation, or "encoding," of memories occurs when the brain engages with new information – ideas, actions, or images – and leads to the formation of a representation of this information in the brain. Sleep preps the brain so that it can assimilate this new information and lay down the framework for new memory traces. Without sufficient sleep – in particular, the slow wave sleep that occurs during the stage of non-rapid eye movement, or NREM – the brain's ability to receive new input is markedly impaired. This phenomenon has critical implications in students and has been observed when college students who were deprived of sleep experienced dramatic deficits in their ability to learn new information.
Sleep facilitates information storage
Sleep also facilitates the more permanent storage of new information that has been stored in the hippocampus – the region of the brain responsible for the formation and consolidation of short-term memories. Sleep that occurs after exposure to new information fulfills the role of the brain's "save button."
Poor sleep, however, inhibits the brain's ability to form memories. Dr. Walker and his colleagues believe that this might be a quality of a time-limited capacity for hippocampal storage. Wakefulness that exceeds the typical 16-hour day might effectively outstrip this region's capacity for short-term storage of information.
Sleep provides a mechanism for information transfer and the formation of long-term memories
The intake and storage of mere short-term information are insufficient for optimal learning, however. The final, and perhaps most critical, way in which sleep aids in learning is that it provides a mechanism by which new information can be permanently stored – the formation of long-term memories via transfer to the brain's cortex, where they can be retained and then retrieved for future use. Without this transfer phase, we run the risk of hippocampal-associated memory impairment – a problem readily observed in older adults who experience loss of slow-wave sleep and subsequently demonstrate difficulty retaining memories overnight.
A fascinating new strategy to selectively enhance memories during sleep
When we sleep, memories and their associated events acquired during periods of wakefulness are reactivated. Essentially, the brain "replays" the events that occurred prior to sleeping, a process that stabilizes memories by serving as a pruning mechanism, selectively strengthening strongly associated memories and weakening weakly associated ones. A surprising fact is that this process can be amplified by "cueing" the reactivation during sleep with sub-awakening threshold sounds, odors, or other sensory cues – based on the context of the learning received the previous day.
A common thread between aging-associated loss of slow-wave sleep, accumulation of amyloid-beta, and impairment of hippocampal-dependent of memory
"If you look at how amyloid builds up in the brain, and if you look at the trajectory of Alzheimer's disease, it is a nonlinear exponential curve. It fits exactly what the sleep-dependent model of amyloid clearance would predict." - Matthew Walker, Ph.D. Click To Tweet
The decline of deep, slow wave sleep begins much earlier in life than most people would expect, with losses occurring as early as the late 20s. By the time a person reaches 50, they've lost roughly half of their deep sleep, and by the time they're 80, deep sleep brain waves are almost undetectable, according to Dr. Walker. Small wonder, then, that aging is accompanied by cognitive decline and substantive memory loss, especially in age-related disorders such as Alzheimer's disease.
Sleep disruption is integrally associated with Alzheimer's disease and its pathophysiology, with characteristic changes in sleep emerging well before the clinical onset of the disease. A key player in the development of Alzheimer's disease is amyloid-beta, a toxic protein that aggregates and forms plaques in the brain. Insufficient sleep increases the production of amyloid-beta, and amyloid-beta deposition, in turn, impairs sleep – in a vicious, self-perpetuating loop.
Recent studies indicate that the lion's share of amyloid-beta accumulates in the medial prefrontal cortex – an area Dr. Walker refers to as the "electrical epicenter" for the brain waves of deep, slow-wave sleep – and the severity of accumulation significantly predicts the degree and extent of cognitive decline associated with Alzheimer's. The accompanying loss of deep sleep impairs overnight memory consolidation and retention, further impairing hippocampal-dependent memory consolidation.
Dr. Walker's research suggests that quality of sleep in later life may actually confer a kind of resilience, staving off the cognitive decline commonly associated with aging.
Sleep facilitates the brain's self-cleaning mechanism: the glymphatic system
One of the reasons slow-wave sleep, in particular, seems to be so important is because it facilitates the proper functioning of the glymphatic system, a system crucial for clearing the brain of metabolites and other waste. The glymphatic system comprises a vast arrangement of interstitial fluid-filled cavities surrounding the small blood vessels that serve the brain. These perivascular structures are formed by astroglial cells and expedite the removal of proteins and metabolites from the central nervous system. During sleep, these interstitial spaces increase by more than 60 percent. This allows a "flushing" operation in which waste products can be more efficiently eliminated. The glymphatic system also facilitates the distribution of essential nutrients such as glucose, lipids, and amino acids, as well as other substances, such as growth factors and neuromodulators.
Our biological need for sleep may reflect a need for an essential downtime that enables the elimination of potentially neurotoxic waste products, including amyloid-beta, a toxic protein that aggregates and forms plaques in the brain. During deep, slow-wave sleep, the glymphatic system clears as much as 40 percent of the total amyloid-beta accumulation. A mere 36 hours of sleep deprivation, however, increases amyloid levels by 25 to 30 percent. This fascinating emerging story on a crucial function of sleep is just one more incremental discovery that helps us understand the existence of sleep in the midst of the evolutionary conundrum mentioned earlier. While many things may help us prevent the build-up of amyloid plaques by boosting our capacity for glymphatic clearance — such as exercise and adequate intake of omega-3 — by far, the most important factor is sufficient sleep, especially slow-wave sleep.
Much of this underscores the need for developing non-pharmacological strategies for addressing sleep loss or enhancement of slow-wave sleep. A strong candidate is transcranial direct current stimulation, a non-invasive, brain stimulation treatment that uses direct electrical currents to the brain to enhance deep sleep and improve memory capacity in older adults, and even doubling it in young adults. Other strategies involve auditory closed-loop stimulation – the delivery of tones in synchrony with endogenous slow-wave oscillations in the brain – and slow, rhythmic bed rocking.
Loneliness as a contagion promoted by sleep loss
"We have not been able to discover a single psychiatric condition in which sleep is normal."- Matthew Walker, Ph.D. Click To Tweet
Another, somewhat troubling, consequence of sleep deprivation is that it triggers the onset of a "loneliness phenotype." Lack of sleep induces critical changes within the brain, altering behavior and emotions, while also disturbing essential metabolic processes and influencing the expression of immune-related genes. The end result is that people who are sleep-deprived avoid social interaction. This asocial profile is recognizable by other people, who, in turn, shun the sleep-deprived people in a psychosocial loop that perpetuates in a vicious cycle of loneliness and other mental health disorders.
Impairment of glucose regulation and the promotion of an obesogenic profile
For anyone who habitually tracks their glucose levels, the importance of sleep can quickly become obvious. As Dr. Walker reveals in this episode, even a few days of impaired sleep, particularly loss of slow-wave sleep, manifests itself in a rather remarkable way: a change from potentially good glucose management, to something akin to a rapid onset of pre-diabetes. This is real-world observable.
In fact, sleeping less than seven hours per night has been associated with either having diabetes or eventually developing the condition. The problem is multifactorial. Not only does lost sleep cause our pancreatic beta islet cells that produce insulin to become less responsive to glucose signals, but muscle and other cells also become less responsive to insulin. These adverse changes from sleep loss are then compounded by deleterious alterations in the body's levels of appetite hormones leptin and ghrelin, which lead to, as Dr. Walker terms it, an obesogenic profile of energy consumption as a consequence of potentially chronic sleep loss.
Sleep plays a vital role in maintaining optimal mental and physical health throughout life. Listen to Dr. Walker explain how sleep is critical to our survival.
Learn more in Van Cauter et al. paper Metabolic consequences of sleep and sleep loss
Discussed in this episode…
-
How pulling an all-nighter decreases learning capacity by 40 percent. Study.
-
How sleep is important for long-term memory because during sleep, we shift memories from the hippocampus, the brain’s vulnerable, short-term storage reservoir, and we move them out to the cortex, the brain’s long-term storage site.
-
How sounds, when played at sub-awakening volume and coupled with certain learning can be used to contextually strengthen memories during sleep… a bizarre and fascinating phenomenon. Study.
-
On a similar note, how exposure to odors during learning and then again during sleep can create this exact same selective-enhancement of retention. That's right — smells and even sounds can reinforce memories even while we sleep. Study.
-
We also talk about a possible explanation as to why we do not remember dreams.
-
Dr. Walker's research showing how loneliness is a type of viral social contagion that is promoted by sleep loss, which was demonstrated by experiments that showed people who were sleep-deprived distanced themselves from social interactions, and were, in turn, shunned by other people. Study.
-
We discuss how the amygdala, the brain's emotional center, is 60 percent more reactive after sleep deprivation due to a dampening down of prefrontal cortex function. Study.
-
The effect that genetics plays in anxiety and poor sleep.
-
How the body's fight-or-flight mechanism is amplified in people who have insomnia.
-
The role of daylight during the day and darkness during the night in improving sleep and circadian rhythms and strategies for using this to our advantage.
-
The fascinating way heat can manipulate the production of crucial slow-wave sleep which has been demonstrated by changes as small as fractions of a degree.
-
How shorter sleep duration has been shown to reduce natural killer cell activity to 70 percent of normal, which, due to the function of natural killer T cells, really suggests chronic sleep deprivation may increase cancer risk. Study.
-
How people averaging less than six hours of sleep at night are four times more likely to become ill after being exposed to the flu virus. Study.
-
How poor sleep overall increases sickness rates, impairs glucose metabolism, and even decreases testosterone levels.
-
How people deprived of sleep for 36 hours show an increase in the amount of amyloid-beta found in their cerebrospinal fluid by as much as 25 to 30 percent and the crucial role that slow-wave sleep plays in helping us clear amyloid-beta. Study.
-
The importance of deep, slow-wave sleep, which begins to decline as early as our 20s, ultimately being cut in half by our 50s, and declining even more — to the point that it is almost undetectable by the time we're in our 80s, according to Dr. Walker. Study.
-
Some of the limitations of most sleep trackers when compared to polysomnography, the gold standard of sleep science diagnostic tools.
-
-
How people who sleep poorly tend to eat 200 to 300 calories more per sitting than those who sleep well and overall have more desire for caloric rich food — a phenomenon that, overall, tracks with a generalized pro-metabolic disorder quality that is associated with poor sleep and shorter sleep durations. Study 1; Study 2.
-
How certain dietary macronutrients may differentially affect sleep. Study.
-
How poor sleep disrupts the gut microbiome. Study.
-
How one cup of coffee in the evening can decrease deep sleep by about 20 percent — an amount that Dr. Walker suggests is equivalent to aging by 10 or 15 years.
-
How alcohol may have a short-lived sedative effect, it tends to fragment sleep, and suppresses REM sleep.
-
How Ambien-induced sleep resulted in a 50 percent loss in the learned connections made during the day in a specialized rodent test of neural plasticity, as well as some of Dr. Walker's other concerns about sleeping pill use in general. Study.
Check the timeline tab for an even more comprehensive breakdown of the discussion.
People mentioned
- Eve Van Cauter, Ph.D.
- Molly Crockett, Ph.D.
- Maiken Nedergaard, MD, DMSc
- Marcos Frank, Ph.D.
- Eus JW Van Someren, Ph.D.
- Aric A Prather, Ph.D.
- Peter Attia, M.D.
- Satchin Panda, Ph.D.
Learn more about Dr. Matt Walker
-
Sleep patterns change during human development, especially around age 12 months, when motor skill learning increases.
-
The strongest predictor of motor skill learning is the spike in stage 2 sleep and sleep spindles.
-
One of the key differences in human versus artificial learning is humans' integration and association of facts.
-
MRIs show that pulling an all-nighter decreases learning capacity by 40 percent. Study.
-
The impact of poor sleep on memory formation may be due to time-sensitive limited storage capacity of hippocampus and lack of non-REM sleep. Study.
-
Sleep is important for long-term memory because during sleep, we shift memories from the hippocampus, the vulnerable, short-term storage reservoir, and we move them out to the cortex, the long-term storage site within the brain.
-
MRI scans of rats learning spatial navigation show that their learning experiences replayed during the rats' sleep to create memories. Press release.
-
When sounds associated with specific objects are played during sleep, memory retention of those objects is better. Study.
-
Coupling sound with specific information enhances memory. NY Times article; Study.
-
Exposure to odors during learning and then again during sleep can enhance retention. Study.
-
Fear conditioning with a characteristic cherry-blossom odor was shown to be epigenetically heritable in mice. Press release; Study.
-
Walker theorizes about why non-REM precedes REM: to capture the memories in the cortex for associations and abstractions made during REM.
-
The connections made during REM sleep are the "longshots" of associations, where we find creative insight and solve large problems.
-
Walker gives examples of famous dream-inspired scientific and artistic insight.
-
People recall dreams more often if awakened during or shortly after dreaming.
-
Walker shares his theory about why we don't remember our dreams: they're stored but not readily accessible.
-
Loneliness as a type of viral social contagion promoted by sleep loss. Study.
-
When a person is lonely, their immune function shifts from mainly viral protection to mainly bacterial protection. Study.
-
In studies where animals are deprived of sleep, the animals become anxious, their cortisol increases, and their glucose metabolism is altered.
-
People who were sleep-deprived distanced themselves from social interactions, and were, in turn, shunned by other people. Study.
-
Sleep-deprivation-induced loneliness was contagious: after viewing people videos of people who were lonely, the viewers felt lonely, too. Study.
-
A small change in sleep can predict how lonely you feel the next day.
-
The amygdala, the brain's emotional center, is 60 percent more reactive after sleep deprivation due to loss of prefrontal cortex function. Study.
-
The unique way the effect of serotonin depletion has been characterized through an investigational technique known as acute tryptophan depletion. Relevant studies.
-
The similarity of the neural signature of sleep deprivation to that seen in psychiatric conditions and Dr. Walker's investigation into understanding the relationship between widespread sleep disruption in almost all major psychiatric conditions.
-
Genetics plays a role in anxiety and poor sleep.
-
The body's fight-or-flight mechanism is amplified in people who have insomnia.
-
Cortisol drops and heart rate slows during sleep in people with normal sleep patterns but not those with insomnia.
-
Walker talks about his personal decision to begin meditating to improve his sleep.
-
The importance of well-timed bright light exposure for the suppression of cortisol and maintenance of a strong circadian rhythm. Study.
-
The role of daylight during the day and darkness during the night in improving sleep and circadian rhythms.
-
Modern society's light exposure contributes to poor sleep, with too little light during the day and too much light in the evening.
-
Walker mentions the work of Dr. Satchin Panda. Episode.
-
Tip. Getting 30-40 minutes of bright light in the morning is crucial to establishing circadian rhythms.
-
Tip. Avoid wearing sunglasses in the early morning hours to reduce symptoms of jet lag.
-
Walker identifies strategies for minimizing light exposure at night to improve sleep, such as reducing blue-light (screen) time and turning off lights in the home.
-
People removed from the modern lighting environment slept better, longer, and earlier. Study.
-
Temperature as a powerful sleep trigger.
-
In order to fall asleep, the body's core temperature needs to drop by about 1°Celsius.
-
The San tribe in Namibia regulate their sleep according to thermal cues. National Geographic article.
-
If you lower core body temperature, you can increase non-REM sleep by 10-20 percent. Study.
-
When rats' paws are warm, they fall asleep quicker and stay asleep.
-
Saunas, hot baths, and hot showers induce vasodilation, which moves blood out of the body's core to dissipate heat, lowering core temperature and inducing sleep.
-
Walker mentions the work of Dr. Charles Raison. Episode.
-
The unique quality of certain immune molecules, such as IL-1, to be somnogenic, and the implications this might have for sleep and immune-modulating activities like exercise. Study.
-
When people are deprived of sleep, pro-inflammatory cytokine levels increase, which may have implications for hospital environment.
-
Shortening the amount of sleep people get reduces their natural killer cell activity by 70 percent, which increases cancer risk. Study.
-
The World Health Organization classifies nighttime shift work as a probable carcinogen. Study.
-
People averaging less than six hours of sleep at night are four times more likely to become ill after being exposed to the flu virus. Study
-
If you get only five or six hours of sleep at night, your immune response to a flu shot is cut in half. Study.
-
The unavoidable loss of sleep associated with pregnancy and being a parent, and some of Rhonda's personal experience with the effects, especially a decline in overall immune health and even glucose responsiveness.
-
Poor sleep increases sickness rates, impairs glucose metabolism, and decreases testosterone levels. Testosterone study.
-
Walker posits his theory about the role sleep deprivation plays as instigator of disease primarily through the manipulation of hormonal signals being governed by the autonomic nervous system.
-
How amyloid-beta tends to build up in the region that Dr. Walker identifies as the brain's “electrical epicenter,” critical in generating deep restorative sleep that is itself critical for amyloid clearance and — importantly — the learning and memory often lost to Alzheimer's disease. Study; Alzheimer's-sleep review.
-
How the newly discovered glymphatic system, which is responsible for ridding the brain of toxic metabolites during sleep, was found to be critically involved in the benefits of deep sleep with the cortical interstitial space increasing by more than 60 percent through a shrinking of glial cells, which allows cerebrospinal fluid circulating in the brain to better flush out toxic amyloid-beta protein. Study 1; Study 2.
-
When amyloid-beta protein builds up in the brain, sleep is impaired, which, in turn, impairs hippocampus-dependent memory consolidation and greater build up of amyloid-beta, creating a vicious cycle.
-
How people deprived of sleep for 36 hours show an increase in the amount of amyloid-beta found in their cerebrospinal by as much as 25 to 30 percent. Study.
-
People who are APOE4-positive are at double the risk of having sleep apnea. Study.
-
Sleep apnea reduces deep sleep and causes hypoxic damage to the brain. Study.
-
Some of Dr. Walker's current research focuses, including identifying "vulnerability windows" of sleep loss during a person's life that may make them more susceptible to amyloid-beta deposition later in life.
-
How deep sleep begins to decline during a person's 20s, and by the time a person is 50, they've lost 50 percent of their deep sleep; by the time they're 70, they've lost 95 percent of their slow wave sleep. Study.
-
Circadian rhythms change with age, blunting our bodily responses from signals that help us maintain biologically useful states such as wakefulness or sleepiness.
-
How, by modifying the light in an elderly care home to just increase the bright light during the day and, thus, improve circadian signals, patients experienced better mood and increased scores on activities of daily living and, in Alzheimer's patients, were able to improve an amount cognitive function in patients with Alzheimer's disease that was comparable in magnitude to acetylcholinesterase inhibitors. Study.
-
By modifying the light in a neonatal intensive care unit - especially through the introduction of a dark night cycle, premature infants showed better oxygen saturation, better tolerance to milk, and accelerated weight gain, which was reflected directly by shortened hospital stays. Study.
-
Some of the limitations of most sleep trackers when compared to polysomnography, the gold standard of sleep science diagnostic tools.
-
The unique place REM sleep may hold as a type of built-in emotional palliative care, even being predictive of remission from depression after trauma. Study.
-
The role REM sleep and NREM slow wave sleep together have in overall cardiovascular health by improving heart rate variability (HRV) and resetting what is known as the "baroflex threshold," respectively — essentially, performing a homeostatic recalibration of blood pressure.
-
Sleep is highly evolutionarily conserved across species in spite of obvious drawbacks, suggesting great biological importance.
-
If a person awakes before getting a full night's sleep, they should try to go back to sleep.
-
Walker identifies his four pillars of sleep: depth, duration, continuity, and regularity.
-
Night shift workers experience a degradation in the overall quality of their sleep, experiencing deficiencies in REM and deep NREM sleep, which suggests that, even for the same total time in bed, proper timing matters.
-
A person's individual chronotype – whether they're an owl or a lark – affects success in modern society, but is largely genetically determined.
-
The ratio of non-REM to REM changes throughout the night during sleep with the shift towards proportionately more REM sleep happening progressively towards the end, resulting in a more substantial loss of REM sleep when duration is cut short.
-
Sleeping at a time that is discordant with a person's chronotype can cause loss of REM sleep, which may help explain associative links between eveningness and depression, low mood, and anxiety.
-
Fighting one's chronotype may have increased risk for poor cardio-metabolic health that can be seen in biomarkers such as hemoglobin A1C, C-reactive protein, and more.
-
People who average less than seven hours of sleep are more likely to develop diabetes.
-
-
Poor sleep affects the release of appetite-regulating hormones leptin and ghrelin. Study.
-
-
Not only do people eat more after a bad night's sleep, they tend to eat more starchy or sugary foods.
-
A diet high in simple sugars and low in fiber makes it harder to fall asleep, and sleep tends to be more fragmented. Study.
-
Sleep or circadian disruption perturbs the gut microbiome, especially through the disruption of a delicate balance in the ratio of Bacteroidetes to Firmicutes species making up the gut, in ways that have been associated with increased risk of metabolic disease and obesity. Study.
-
How it may be the ramping up of our body's fight or flight system from sleep deprivation or low quality sleep that induces some of the harmful changes in the microbiota, and how this two-way communication between the gut and the brain may also create an opportunity to use interventions that improve our microbiota to, in turn, improve our sleep.
-
Some of the pre-clinical evidence demonstrating that certain strains like Lactobacillis Rhamnosus have been shown to alter GABA activity in the brain, including regions like the hippocampus and amygdala, via a vagal nerve-dependent mechanism that ultimately suggests promise for conditions involving alterations in the GABAergic system like depression and anxiety. Study.
-
The extremely straightforward relationship sleep loss has on anxiety, where every hour past 14 to 15 hours of wakefulness results in an increase in anxiety in a dose-response sort of manner. Study.
-
Walker identifies some of his top actionable steps for improving what he calls the four pillars of sleep, which focus on improving depth, duration, continuity, and regularity. Continues at 02:17:45.
-
The evidence showing that reading from a light-emitting ebook reader or iPad may have a more significant blunting effect on melatonin than just reading a printed book with reflected light, leading to delaying of circadian phase, REM sleep propensity, and, ultimately, impaired morning alertness. Studies: 1, 2, 3.
-
Excessive smartphone use may also impair sleep through a more generalized promotion of anxiety. Study.
-
Matt's thoughts on the optimal temperature for sleeping (around 63 to 66 degrees).
-
A person shouldn't stay in bed if they can't sleep to reestablish the bed as a place of sleep.
-
One cup of coffee in the evening decreases deep sleep by about 20 percent - an amount that Matt suggests is equivalent to aging by 10 or 15 years.
-
Caffeine has a long duration of action.
-
Alcohol has a sedative effect, tends to fragment sleep, and suppresses REM sleep. Study.
-
Marijuana has variable effects on sleep, depending on the active components.
-
Sleeping pill use is associated with higher risk of cancer and all-cause mortality.
-
Ambien-induced sleep resulted in a 50 percent loss in the learned connections made during the day. Study.
-
Sleeping pill use was associated with a higher risk of death and susceptibility to infection. Study.
-
The American College of Physicians no longer recommends sleeping pills as a first line of therapy for insomnia.
-
Most medical doctors receive fewer than two hours of sleep education during medical school.
-
Walker has written a book called Why We Sleep.
-
Walker can be found on Twitter at @sleepdiplomat and on his website at sleepdiplomat.com.
Rhonda: Today's guest is Dr. Matthew Walker, author of New York Times best selling book Why We Sleep: Unlocking the Power of Sleep and Dreams, Professor of Neuroscience and Psychology at University of California Berkeley, and Director of the Center for Human Sleep Science.
YOU WILL NOTE… This episode starts sort of abruptly. The opening discussion is about HOW SLEEP PATTERNS CHANGE DURING HUMAN DEVELOPMENT, especially around age 12 months, when motor skill learning increases.
Matt and I had planned on doing an intro but the camera was rolling and the discussion was so interesting that we just kept going.
This is a good one, folks. Enjoy!
Matt: What's really interesting is if you look at sort of sleep, and we've done some of this work, and I maybe will speak about it on sleep and motor skill learning, and that seems to be more dependent on this sort of lighter form of non-REM sleep Stage 2 and particularly the burst of electrical activity the sleep spindles, there's a really bizarre bump in Stage 2 and sleep spindles during development, it happens right around the 12-month period, which is where, all of a sudden, you start to see considerable limb or multi-limb coordination. In other words, you start to perambulate, you start to learn how to walk.
It's almost as though there's like a homeostatic response, which is that with the drive for motor plasticity and learning comes a response from sleep to say, "Oh, now we're into motor skill learning? We need to consolidate." And you get this...it's a really strange bump, and it dies away again after the...
Rhonda: What's the sleep, the spindles, sleep two spindles, what stage is that?
Matt: Well, you see sleep spindles throughout almost all of non-REM. So once you get past the lightest sort of Stage 1 on REM, then you get spindles throughout all of non-REM, but they are a prototypical feature of Stage 2 non-REM as well. Then Stage 3 and 4, which is sort of like the deep sleep stuff, you also get spindles there, too. But in our hands, at least, the strongest sleep stage and the strongest electrical signature in your EEG that is predictive of your motor skill learning is Stage 2 and sleep spindles, both of which seem to have this bizarre sort of, you know, coincidental spike right around this developmental phase of crawling, standing, walking.
Rhonda: Yeah. So many things going on during the development. I mean, it's so fascinating to observe for sure.
Matt: And language, too. I mean, when we've looked at this as well with teaching adults foreign languages, or even actually just mathematical languages or artificial grammar, sleep is a huge component in that. But they also saw this fascinating thing with development, which was about not just concrete learning of individual facts but the generalization of knowledge.
So this is sort of the thing that I think separates us from computers, at least for now, which is that computers are very good at storing individual bytes of information in a vertical way very clearly. And we can do that, too, storing individual facts. But what computers don't do, which is what we do, is intelligently integrate and associate them together so that we can extract overarching patterns and schemas and statistical rules about this thing called the world in which we live.
And, yeah, sorry, I was just gonna say that you can, with infants, you can teach them just these novel sounds, and each one of these strings of sounds is unique and different. But there's something common about the grammar that is binding and overarching across all of them. There is an overarching schema that you could learn in addition to each one of the individual facts.
After they've had a nap versus an infant that has not had a nap, post-nap, the infants have extracted and understood the generalized rules of what they've been learning, not just the individual facts. Whereas infants that have learned but haven't napped have not sort of made the abstraction.
Rhonda: So my being a nap nazi, I should be rewarded for that, right?
Matt: Absolutely.
Rhonda: It's absolutely like...
Matt: And it stays from the, you know, infancy all the way through to adulthood. So if you're napping, I'm not gonna...well, there's a few double-edged sword aspects of napping.
Rhonda: So I wanted to ask you a question, you're talking about basically being able to connect the dots, you know, how would that sort of differentiates us from what a computer can do, I mean, one of the things. But is there a certain...I remember reading in your book, and this is probably the part of the book that I was more skimming, you know, like...and that was the importance of REM sleep and dreaming and creativity. So is that, connecting...because I feel like connecting the dots, you know, requires some creative thought to be able to kind of, like, put things together and come up with a big-picture idea and figure things out. So is it known? Is REM sleep important for that?
Matt: Yeah, it does seem to be. So if there is...So, I mean, we could take a step back and think about how does sleep achieve memory processing, learning, information processing. And sleep seems to be important in at least three ways. First, you need sleep before learning to actually get your brain ready to initially soak up new information, to initially lay down new memory traces.
But you also then need to sleep after learning to take those freshly-minted memories in the brain, particularly in a region that we call the hippocampus, which you could think of almost like the informational inbox of your brain, but it's very good at receiving those sort of new memory files. But you need sleep after learning to take those new memories and then essentially hit the save button on them so that you don't forget those informational pieces of the puzzle. So sleep before learning to get your brain ready, to acquire information. Sleep after learning to hold on to those individual facts.
Rhonda: So let me get this straight. So if you want, for example, short-term memory, right, because if you're sort of wanting to store things in the hippocampus, even short-term, that would be sleep before.
Matt: That's right.
Rhonda: And then if you want to then consolidate it and have a long-term memory, that would be your sleep after?
Matt: Sleep after.
Rhonda: Okay.
Matt: So you can't cheat sleep on either side of the memory equation. You've got to...You can't pull the all-nighter and hope to be able to continue to learn. And we did this study. We said sort of, you know, "Is it wise to pull the all-nighter before the exam?" So we took a group of individuals, assign them to one of two groups, a sleep group and a sleep deprivation group. A sleep group, they get a full eight hours of shut-eye that we measure here at the sleep center. The deprivation group we keep awake all night under full supervision. And they don't get any naps. There's no caffeine. It's miserable for everyone involved.
Rhonda: Wow. No caffeine.
Matt: No caffeine at all. And then the next day, we place them inside an MRI scanner, and we had them try and learn, and cram, essentially, a whole list of new facts into the brain, into the hippocampus. And the first result was that the sleep deprivation group was about 40% more deficient in their learning ability. So they learned 40% less, four zero, which is...
Rhonda: That's astronomical. That's a huge...
Matt: Non-trivial. I mean, if you want to put that in context, I guess it's the difference between acing an exam and failing at miserably 40%. What was interesting, though, is what was going on in the hippocampus, this informational inbox of the brain. When we looked at that in those people who'd had a full night of sleep, you saw lots of healthy learning-related activity. It was beautiful.
In the sleep deprivation group, we actually couldn't find any significant signal whatsoever. And so it was almost as though sleep deprivation had sort of shut-down-your-memory inbox and any new incoming files were being bounced. And we put forward a theory as to why that was. Perhaps that the hippocampus being a short-term reservoir of memory has a limited storage capacity, perhaps a little bit like a USB stick.
And you have maybe, in humans, a 16-hour recording capacity for information acquisition before you have to sleep. Because it's during sleep, then after learning. So that's sort of the story before learning. It's not great. We can show it. We know in the brain what part of the brain is failing to produce those impairments.
Rhonda: In that study, you were testing the ability to acquire new information.
Matt: Exactly, to sort of lay down those fresh memories and just to grab hold of them. And you can't do that well without sufficient sleep. And that seems to be in part related to your non-rapid-eye-movement sleep or your non-REM sleep.
But then, what we've also done in lots of these, and we and lots of other people have now replicated this finding, sleep after learning then takes those memories and it sort of it hits the save button on them. It's a little bit crass. Actually, what really happens is that during sleep, there is a file transfer mechanism that takes place at night, that we shift memories from that short-term vulnerable storage reservoir, the hippocampus, and we move them out to the long-term storage site within the brain, which is the cortex, which essentially acts like a hard drive.
And that means that when you wake up the next day, there are two delightful benefits. First, having shifted those memories from the short-term vulnerable reservoir to that more permanent sort of safe storage haven in the brain. They're protected, and they're safe, so that you're going to remember rather than forget.
The second benefit, however, is that sort of having cleared off those files from the hippocampus, almost like shifting files from the USB stick, you've cleared out all of that fresh memory encoding reservoir, so that when you wake up the next morning, you can start acquiring new files all over again. So it's this sort of elegant, symbiotic system of memory that happens.
Rhonda: Yeah, beautiful.
Matt: Yeah, absolutely. Sorry.
Rhonda: We'll, of course, use all this.
Matt: It's hermetically sealed. It's bizarre.
Rhonda: I remember reading somewhere that when you sleep, and this is related to what you were just talking about, that your brain sort of replays, like, electrical-activity-wise, it looks like you're literally, like, reliving the same thing you just learned or something. Is that...
Matt: That's absolutely correct. So these studies firstly happened in animals, and we've now been replicating some of them with brain imaging, with MRI scans in humans. Hard to believe, but we can do it. But the original findings were fascinating. They would place electrodes into that structure that we spoke about, the hippocampus, which also rats have as well, and it helps rats learn spatial navigation.
And they would place lots of electrodes into this part of the brain. And as the rat would run around the maze and learn the maze, individual cells would fire, and they would spatially code which part of the maze the rat was in. So different cells are mapping different parts. It's like sort of navigating a route from your home to work. Different sort of cells are coding the journey along the way.
Rhonda: Yeah. I'd probably would suck at doing that, but...
Matt: I think, yeah, yeah. I lost that. Yeah, some people say it's a male aspect of the gene, but I definitely lost it. Anyway, but what is delightful was that you could sort of hang, you know, a sound tone on each one of these electrodes. And what you would hear, and this is just, you know, for audio, you would hear sort of "buh buh buh bump, buh buh buh bump, buh buh buh bump," as the rat was running around the maze, as these cells were learning, encoding, and creating this kind of memory circuit essentially.
And, yeah, you know, "buh buh buh bump," off it goes. But what was genius is that they kept recording. And as the rat fell asleep, what did they hear? And it wasn't just static random firing, which is what we thought typically happens during sleep. In that static of electrical impulses at night, in a sea of electrical noise, came out a very clear, predictive, message, which was "brrrmp, brrrmp, brrrmp." It was exactly the same temporal sequence "buh buh buh bump, buh buh buh bump, buh buh buh bump," but it was sped up. And we now know that it's during sleep that we replay, but we replay at somewhere between 10 to 20 times the speed.
So it's as though you're kind of, you know, you've done the, you know, recording of whatever happened during the day, but then it gets replayed but at times 20 or times 10. "Brrrp, brrrp, brrrp, brrrp, brrrp."
Rhonda: Wow. So is this is a long-term potentiation part? Is this where it's solidifying?
Matt: Yeah.
Rhonda: Now what stage of sleep is that? I know you mentioned...
Matt: So that's during deep non-REM sleep.
Rhonda: Deep.
Matt: Yup, that we see that.
Rhonda: It's the sleep I'm always trying to optimize for, and it's just so difficult.
Matt: And it's difficult, you know, I think...Well, sleep in general is difficult for so many people, and we can speak why. So this starts to come back to your original question about REM sleep, though. So we get this memory replay. It's absolutely fascinating. We can now see it in humans. We can even manipulate it, which is amazing.
So if I teach you some information on a screen. Let's say it's about a particular object, like a fire engine, and you have to try and learn both the object and the spatial location of that on a screen. And then tomorrow, we're going to sort of come back. And I'm just going to show you the image and say, "Do you remember seeing it or not, yes or no?" And if you do remember seeing it, you've got to place where you thought it was on the screen. So you have to learn the item, and you have to learn the associated location.
But here's the great part. During the initial learning session, before you slept, not only do you see the fire engine but we play the sound of the fire engine, like a fire engine ring. And then we show you a kettle. It's whistling. We show you a cat. It's meowing. So each of these items that you're making has a contextual cue associated with it, a sound. And it's a congruent sound, fire engine sound, fire engine, kettle sound.
And here's the fun part. I can teach you a hundred of these items, and then during sleep, I'm going to replay those sounds that you heard as if I'm trying to get into your brain and I'm selectively reactivating each one of those individual memories. But I'm only going to reactivate and replay half of those memories. I'm gonna go to replay 50 of 100 things that you've learned.
And then the next day, we wake you up, and we test you. And firstly, your memory is better after sleep. And that's what we found. What's interesting is that for those items that I replayed during sleep, they are almost twice as superior in terms of your memory retention.
Rhonda: So the playing of them doesn't disrupt the sleep at all or...?
Matt: Well, that's the key. You have to play at a sub-threshold-awakening sound. So we will test your auditory threshold, and we will then play the sound at a level that we know is below your awakening threshold. So it's still just enough to get in to penetrate into the brain and tickle the memory and reactivate it...
Rhonda: That's fascinating.
Matt: ...but it's not enough to wake you up. So now, you know, you could imagine, you know, I've got these science fiction ideas of thinking, well, I learned all of this information, and maybe I can just put my favorite playlist on, you know, at night at low sound and, you know, stimulate these memories. Or could it be a study aid where you, you know, help students, like, sci-fi stuff?
Rhonda: So you think coupling different sounds maybe with, you know, learning facts, it may actually help...
Matt: Yeah.
Rhonda: Like irrespective of replaying them, like, during sleep, do you think just even the coupling of the sound somehow can help, can remember your...?
Matt: As long as those sounds have been coupled and bou to specific information. And this is what we call context-dependent or key-dependent memory. This is well known in psychology over about 100 years. If you study in the room that you're going to take the exam, you do better, because you actually use cues, contextual cues from around the room that are triggers to help you better remember.
Rhonda: Wow.
Matt: We're just doing that with sleep.
Rhonda: What about caffeine? So if you study caffeinated and you don't take your exam caffeinated. Is this kind of the same concept?
Matt: We don't know about caffeine. It's an interesting thing. Caffeine may be a...it's a nonspecific stimulant, whether it works with ingested substances. We know, however, this works also with odors. So have you ever had that experience where you're sort of in an airport and you're sort of tying your shoelaces at the security, someone walks past with that cologne or a perfume of a person you knew, and it instantly unlocks that memory, as if the sound has triggered the reactivation of the memory, and it comes flooding back.
Well, you can do the same thing with this memory and sleep trick, where I teach you stuff during the day, and we can puff certain odors up your nose and associate the smell with the learning material. And then during sleep, you reperfuse the odor up the nose...
Rhonda: Oh, really?
Matt: ...and you can get the same benefit as well, the same doubling of the benefit.
Rhonda: Wow, that's fascinating. I remember this study that was done, that was coupling an odor, it was like a cherry blossom odor, with an electrical shock. So those, you know, classical fear studies that they do in mice, it was in rodents. And there was some sort of epigenetic change that the breathing of the odor, or the cherry blossom, was inducing. That was like changing some receptor on the glucocorticoid receptors. So it was getting passed on to, like, the next generation. And so even though the next generation didn't have the shock and the coupling of the smell, you know, if they were exposed to the smell, they have the fear.
Matt: The critical memory was translated from one generation to the next.
Rhonda: Yeah. So, anyways, it'd be fascinating. You don't know what role sleep plays in the epigenetic transfer.
Matt: Right. So if we all start doing this, you know, are our children going to be incredible memory replayers, you know, by the way of...But to come back to your...I'm sorry I've taken a desperately long time to answer your original question, which was what about REM sleep.
So what we've spoken about is the first two of the three stages of memory processing with sleep, sleep before to get the brain ready to lay down memories, sleep after to grab a hold of those individual memories and cement them into the neural architecture of the brain. Once you've done that, though, there's a final step. And that seemed to not depend on deep non-REM sleep but instead depend on rapid eye movement sleep or REM sleep, which is what most of us know as dream sleep.
And it's during dream sleep that your brain essentially performs informational alchemy, is what I would describe it as. It's a little bit like group therapy for memories that sleep has gathered in all of the information during the day. And during non-REM sleep, which always comes first, by the way, in our sleep cycle. We always have non-REM sleep first, then REM sleep second, then non-REM sleep again, then REM sleep second.
And we don't know why there is no good explanatory data suggesting why non-REM sleep always comes first and REM sleep comes second. But I've put forward the theory that, for information processing, it makes sense. Which is that non-REM sleep first to just get what you've learned and lock it into the brain. REM sleep then comes along, and REM sleep starts to fuse all of the information that you've recently learned with the entire back catalog of information that you've got stored up across a lifetime of experience.
And it's this sort of...Essentially, REM sleep is creating a revised mind wide web of associations. And I'd like to sort of think of what's going on with REM sleep. And we've done lots of these studies to look at this and these clever ways that you can look at sleep and associative memory processing and building new novel connections. And it's almost like memory pinball, where you take these new memories and you sort of launch them up, and you start bouncing them around into the architecture of information within the brain. And you're starting to test associations. You're starting to say, you know, "Should this new information be connected to this? Maybe not. Should it be connected to this? Maybe not."
Now some of that happens whilst were awake during the day. We make obvious connections. But what's strange is that we make connections during REM sleep but they're not of the same kind. The connections that we're making during REM sleep are the longshots. This is the bizarre...
Rhonda: The bizarre, right.
Matt: ...strange. You know, it's sort of...it would be the equivalent of saying, during the day, we take this information, and the connections we make are like a Google search gone right, which is the first page is all of the things that are most related. And it's very obvious. Page 1, that's directly related to what I inputted.
During REM sleep, it's almost as though you input the search term and you're immediately taken to page 20 of the Google search, which is about some field hockey game in Utah. And you think, I don't understand. Oh, that's interesting. I see what you're talking about. So we make these bizarre leaps of associative memory processing faith during REM sleep. And that's why we now understand that it's REM sleep that helps us divine remarkable creative insights into previously impenetrable problems.
And you can see this throughout the history of human beings, this dream-inspired insight, scientific demonstrations. You know, August Kekulé divined the idea of a benzene ring, these double carbon rings by dreaming of a serpent that swallowed its tail. Dmitri Mendeleev, you know, came up with the Periodic Table of Elements by way of dream inspiration. And, you know, people have won Nobel Prizes, Otto Loewi won the Nobel Prize for the demonstration of chemical transmission across nerve cells. And he dreamt of the experiment that helped improve that. He didn't dream of the concept itself, but he dreamt of the experiment to prove it.
Wonderful, artistic demonstrations of this, too. You know, Paul McCartney has written innumerable songs, it turns out, by way of his dreams. Keith Richards came up with the opening chords of Satisfaction by way of dream-inspired insight.
So REM sleep takes that third component of information processing. And I think it's what defines us differentially from computers in part, which is that deep sleep is about knowledge, which is gathering all of the information and holding on to it. REM sleep, I would argue, is about wisdom, which is knowing what it all means when you fit it together, you know. That's what I want from a good student. Don't just give me dry-book learning. Do you really understand it? Can you apply it? Are you creative? That's dream sleep.
Rhonda: Right, a deep thinker. Why do you sometimes not remember your dreams and sometimes you do remember your dreams? Do you have any idea?
Matt: Yeah. So some of it seems to be about, if you wake up out of that dream sleep period and then you go back into sleep, the awakening can sometimes help you commit that experience to memory.
Rhonda: Oh, okay.
Matt: But there are people who say that I never remember my dreams, you know. We can bring those people into my sleep center, and we can, you know, wake them up in the middle of dream sleep, and they'll say, "It's remarkable. For the first time, I was dreaming." And the answer is no. It's not the first time that you are dreaming. It's just the first time that you've actually remembered a dream, because it's the first time you've typically woken up.
Rhonda: Okay. My mother-in-law, you know, claims that she doesn't dream. And, of course, I'm like, "No, you have to dream."
Matt: Yeah.
Rhonda: That must be...
Matt: There are a selection of patients that have a lesion in a part of the prefrontal cortex, in their white matter, which are these big sort of informational fiber tracts that communicate impulses. If you get a lesion deep down there, we do seem to genuinely see a cessation of dreaming in those patients.
By the way, I would...I didn't even feel confident to write this in the book, and it's still a theory that I've never really heard in public, but go with me on this. Which is, I think that we may actually remember all of our dreams, or it's possible that there's a tenable theory. The problem is we don't have access to those dreams. Those dreams are memorized, and they are available. They're just not accessible. I think what happens as we wake up is that we lose the IP address to those memories. And the reason I believe this to be potentially true is have you ever had the experience where you wake up and you think, I was dreaming, and I know I was dreaming. And you try as hard as you can. The harder you try, the...
Rhonda: Yeah.
Matt: ...worse the memory-recall goes? And then you think, forget it. Two days later, you're walking along, and you see a street sign, and all of a sudden, it triggers the unlocking of that dream memory. You think, oh, that's what the dream was about.
As a neuroscientist, that tells me that the memory was present. The memory was available. The problem was accessibility. You couldn't gain recall access. So the information is there. It's just not accessible. If that's true...
Rhonda: It's happened to me just even after I've, you know, when I go to bed. You know, later that night, I hit the pillow, and all of a sudden, I remember the dream right as I'm hitting the pillow.
Matt: Right.
Rhonda: That's happened to me more than once. But you're right.
Matt: Right. It sort of tells you that there is...it's almost a scary prospect, which is that maybe every single one of our dreams throughout life are stored and are present and determine our behavior to some degree, because we know that there is an enormous amount of information that changes our behavior or decisions that goes on below the radar of consciousness, implicit memory. That could be true for dreaming, too.
And I think I've got an experiment that we may be able to design to actually get at this. And if that's true, it should, hopefully, radically change our view of dreaming, that dreams are ephemeral, that they dissolve quickly, they're forgotten, and they don't influence us as human species.
Rhonda: That would be pretty groundbreaking.
Matt: Yeah, we'll see.
Rhonda: You just had a study that I just read, I think, yesterday on sleep and it affecting behavior, loneliness, or...
Matt: Yeah, so we just published a sleep study demonstrating that sleep loss will trigger viral loneliness. And it was a three-part study. I mean, firstly, the reason that I got into this was loneliness is a killer. We know that there is a massive epidemic of loneliness now in industrialized nations. Being lonely increases your mortality risk by about 45%. In other words, being lonely is twice as risky for your death concern than obesity...
Rhonda: Wow.
Matt: ...which is striking.
Rhonda: Yeah. There was actually a study showing loneliness changes, like, a massive amount of gene expression and, like, up-regulates NF-kappaB, cortisol, like all these pro-inflammatory genes. So it makes sense that it'd be associated with...
Matt: And what's bizarre about loneliness...By the way, I'm taking a complete...this has got nothing to do with sleep. But if you look at the profile of your gene expression and your immune system, you've got some immune components that will go after viruses. And viruses can only be transmitted from one human being to another by way of touch. They can't live outside of our bodies. Bacteria, so if you scrape yourself on a fence, like, you know, walking past it, you can get a bacterial infection because bacteria can live outside of the body.
When you become lonely, your gene expression shifts you away from a profile of immunity that normally deals with viruses and pushes you to more towards a bacterial defense profile.
Rhonda: Really?
Matt: Isn't that incredible?
Rhonda: Yeah, you should send me that study.
Matt: That your psychology...
Rhonda: Yeah, that's fascinating.
Matt: And there's a couple of folks at UCLA, who, if you ever have interest in this area of how loneliness, the mind, the mood...
Rhonda: Oh, totally. Yeah.
Matt: Okay, I've got to give you these people. I'm a complete fan of...
Rhonda: Please do.
Matt: ...their work. And they did this study. And it just blew my mind. How could a concept that is so sort of, you know, out there, and some people almost don't, you know, believe in loneliness. Toughen up. What's wrong with you? Go out make some...How could that change the expression of your genes and even alter how you, the organism, fend for yourself from an immunological perspective shifting you from viral to bacterial defense. But, anyway...
Rhonda: Wow.
Matt: So coming back, I was desperately concerned about the state of loneliness. What's interesting, I was reading a lot at the time, because we do a lot of work with sleep and psychiatric disorders including anxiety, and when I was reading the studies where they would take animals and they would deprive them of sleep, you've got this anxiogenic profile where you got cortisol increasing, you got shift in insulin and glucose regulation, all of the bad things that you would not wish to happen, an anxiety increase, they had fear-like behavior all by way of just sleep restriction.
But what was also interesting is that sometimes the researchers would note, despite not measuring it systematically, that the animals, who would often be secluded by themselves in the cage, even when they were with other conspecifics, and other conspecifics would not approach them either.
Rhonda: Okay.
Matt: And so it seemed to me just from reading this, I thought, well, this seems like an animal phenotype of human loneliness. And it seems to be caused by a lack of sleep. So we decided we had to do the study.
So the first part of the study, we took a group of individuals, and they went through the study twice. They were either deprived of sleep for an entire night, or they got a full eight hours of sleep. The first test was, do you have a social repulsion boundary, and that boundary is increased when you are sleep-deprived. So I think everyone has that sense that if I start moving closer to you, you think, okay, do you know what, at some point, that's kind of enough. That's about my close distance.
What's interesting is that if I ask a sleep-deprived an individual to stay put, and I ask you, as an experimenter, to walk towards the sleep-deprived individual, and the individual says, "Stop," when they feel comfortable relative to when that very same individual has had a full eight-hour night of sleep. When you're sleep-deprived, you decide to push people a further distance away from you. So you have a lower desire for social proximity and social interaction.
Second, we then replicated that finding, but now we had them inside the MRI scanner. Because we wanted to see what was changing the brain to produce this social repulsion. What we found was that the regions of the brain that are essentially an alarm network, which is a sort of a stay-away-from-me network that is sort of in the parietal cortex and the premotor cortex, it's sort of what we call the near space network. So it creates your comfort of boundary. And when objects start to approach you, it alarms to say, "Incoming. Be cautious. Be wary." That part of the brain became hyperactive when people were sleep-deprived...
Rhonda: Wow.
Matt: as if you were getting this repulsion signal from the brain. If that wasn't bad enough, the other parts of the brain that have been called the theory-of-mind network, which sort of helps you understand the intent of other people, it's a pro-social network in the brain, it cooperates pro-social interaction, that part of the brain was shut down by sleep deprivation. So it's a double-edged sort of sword.
So we weren't satisfied with that. Next, we wanted to say, "Could someone who just looked at these sleep-deprived individuals, could they actually judge them as being lonelier and looking lonelier and beaten, sort of perceived as lonely, even though they knew nothing about the experiment?"
So in the experiment with the sleep-deprived individuals, we also did videotaped interviews with them. And we just asked them general questions. Tell us about a movie that you watched? Or what was happening in the news this week? Just bland stuff. And then we got 1,000, I think was it was over 1,000 people, 1,083 people online. And they knew nothing about the experiment. They didn't know it's about sleep, sleep deprivation, knew nothing.
And we showed them just a 60-second clip of these people when they'd have a good night of sleep and when they were sleep-deprived. And we just asked them, "How lonely does this person appear to you?" And they knew nothing. But despite knowing nothing, they consistently and reliably rated the sleep-deprived version of the individual as seeming lonelier.
We also asked them, "Would you socially interact with this person? Would you friend them on Facebook? Would you work with them in a business environment?" And they consistently rated that they would prefer not to engage and interact with them.
Rhonda: Is that because they just looked unhappy or looked...?
Matt: Well, we actually think it's a collection of things. It's that their appearance, but also their vocal tone, is very different. We think there's a lot of...This is now one of the key things. What's communicating this asocial profile?
Rhonda: Oh, so they are listening to them speak?
Matt: So they watched them, and they listen to them speak. So they could hear them as well. So we demonstrated that. There was, unfortunately, the social repulsion on both sides of the equation. When you're sleep-deprived, you yourself don't want to have anything to do with other people. And that perhaps wouldn't be so bad if people would only at least come to your rescue, because they would see you in need. The opposite is true. People find you socially repulsive as a consequence. So there's a push from both sides of the social dyad.
The next thing, we asked those people who were rating the sleep-deprived individuals, we also said, "Look, how lonely do you feel after just the 60-second clip?" And they themselves felt lonelier after interacting with sleep-deprived individuals. In other words, this contagion of sleep-deprivation-induced loneliness.
Rhonda: So I wonder how much of this can be translated to, like, someone that, say, for example, gets only five or six hours of sleep versus, of course, not getting a full night sleep. You know, maybe there's, like, a little, just a little bit of this penetrating...
Matt: We then asked that question. That was the final part of the study, which is that we said, "Okay, this is extreme sleep deprivation, and most of the population does not undergo this. What about a more ecological version?" So we tracked hundreds of people across two nights of sleep. And we asked, just by a subtle variation of nature, our small perturbations of sleep from one night to the next, do they predict how lonely you experience yourself to be from one day to the next? And these are small minute changes in sleep efficiency, just small reductions in sleep of tens of minutes.
Lo and behold, even just that small change in your sleep from one night to the next, we could measure, predicted how lonely you would experience life the next day from one day to the next. So it doesn't even take, you know, two hours of sleep reduction.
Rhonda: Wow.
Matt: Small minutes.
Rhonda: I remember reading somewhere, too, that isn't the, like, amygdala, like hyperactive or something happens, there's not an inhibitory signal that occurs if you're sleep-deprived or...?
Matt: That's right.
Rhonda: Is that correct?
Matt: Yes.
Rhonda: So then you're feeling more...you're, like, alarmed and, you know, just anxious and feeling that in a, say, threat...
Matt: That's right.
Rhonda: ...that ongoing threat that really isn't there.
Matt: Exactly, yeah. So we published the study in 2007 where we, again, sort of sleep-deprived people, put them inside an MRI scanner, and we showed them increasingly negative and aversive and unpleasant images. And what we saw is that, relative to people who'd got a full night of sleep, the amygdala, this sort of emotional epicenter for the generation of strong, emotional, impulsive reactions, that deep emotional center was 60% more reactive under conditions of a lack of sleep.
And then we asked why. Why is your emotional brain so sort of sensitive and erupting with such extraordinary activity? And what we then went to find, or went on to find out in later work, was that another part of your brain called the prefrontal cortex that sits directly above your eyes here, and particularly the middle part right between your eyes, that part of the brain acts almost like the CEO of the brain, of your emotions, and your hedonic impulses. And it sends sort of an inhibitory top-down regulatory control. It's sort of, like, the brakes on the gas pedal of your emotions.
That part of the brain was shut down by sleep deprivation, and you'd lost that communication to the amygdala. So now you, from an emotional standpoint, you were all emotional gas pedal and too little regulatory control brake as it were.
Rhonda: It's really interesting. This work kind of reminds me of...I'm not sure if you're aware of any of this research. A lot of it has been done by Dr. Molly Crockett, who, I believe, now she's at Harvard. But she has done a lot of studies looking at serotonin depletion in the brain. And basically, you can induce that by giving acute tryptophan depletion, giving someone like branched-chain amino acids to compete with transport for tryptophan in the brain, which then basically drops serotonin levels. I mean, you can drop your serotonin levels down to, like, 10%.
Matt: And mood is...
Rhonda: And the same thing happens where, exactly what you were describing, the inhibitory signal that happens from the prefrontal cortex onto the amygdala is, like, stops. And so people become extremely impulsive. Terrible moods, a little more aggressive, their long-term planning shuts down, and they just, like, going for the short-term gratification. Very similar. So it'd be kind of interesting...I don't know how serotonin would be related to all that, but there must be some sort of connection.
Matt: Yeah. I mean, and I think there's a number of different, I think, neuro chemicals that can produce that same kind of neural phenotype and as it were. But what struck me was that when I looked at that neural signature of sleep deprivation for the emotional brain, it was not dissimilar to numerous psychiatric conditions. And that then now, gosh, 11 years ago, I'm showing my age, but that set sort of, you know, the sleep center off on a completely new trajectory of work. And we're doing a lot of this work in sleep and psychiatric disorders.
And I think one of the most fundamental things that I can say at this point is that we have not been able to discover a single psychiatric condition in which sleep is normal. And so I think sleep has a profound story to tell in our understanding, maybe our treatment, I don't know about prevention, but possibly, of grave mental illness. And psychiatry has known this, by the way, for, you know, 40 or 50 years. It's always been documented that sleep disturbance goes hand-in-hand with psychiatric disturbance.
Rhonda: Maybe there's some sort of complex gene environment interaction. A few people that are more genetically susceptible and are getting...losing the sleep, or, like, the ones that are kind of pushed into a disease state.
Matt: And we've seen this, too, that if you look at that emotional brain reaction signature that I just sort of described, and you repeat that, but with people who are high-anxious and low-anxious, and we know some of the genes that are associated with being high-anxious and low-anxious. So we're using anxiety as a sort of a proxy for perhaps a particular genotype here. What you see is that it's those high-anxious people who are the most vulnerable to this impact of a lack of sleep. Those who are low-anxious still have a bad outcome, but it's nowhere near as bad. So there seems to be sort of interactions here between sleep loss and your basic trait levels of being sort of a nervous, anxious type to begin with.
Rhonda: That makes sense.
Matt: And those are the people who are, sadly, the people who typically don't get a good night of sleep anyway.
Rhonda: Right. So you're saying anxiety is, like, one of the things that stops me from sleeping.
Matt: It's the principal trigger of insomnia.
Rhonda: Yeah, really, true.
Matt: It's the model of insomnia right now, is that you get...And if you look at the nervous system, that's how we understand insomnia right now, is that its principle is...I think ultimately we'll find that there are multiple flavors of insomnia, different forms. We already categorized two of them. We've got what we call sleep onset insomnia and sleep maintenance insomnia, difficulty falling asleep, difficulty staying asleep. They're not mutually exclusive. You can have both, or you can just have one or the other.
But coming back to it, I think the overarching biological red thread narrative of insomnia is an amplified fight-or-flight nervous system, that your nervous system is split into these two branches, what we call sort of the sympathetic and parasympathetic parts of your autonomic nervous system. The sympathetic is anything but sympathetic. It's poorly named. It's the fight-or-flight branch of your nervous system. It ramps you up, charges you up, releases cortisol, adrenaline.
You constantly see an overactive, sympathetic nervous system in people with insomnia. And when you measure their cortisol across the 24-hour period, in most of us, just as we're getting to our natural bedtime, cortisol just starts to now drop down. We start to see that cycling down of cortisol. The opposite happens in people with insomnia. You get a continued rise right around that bedroom period. And it seems to be very predictive of sleep onset problems.
If you look throughout the night, cortisol then starts to plummet, and it drops beautifully down. It's part of the reason why deep sleep is the best form of natural blood pressure medication that you could ever wish for. Your heart rate drops down, your vessels relax, cortisol drops down. But in other insomnia patients, we see this bizarre spike in cortisol in the middle of the night. And it predicts nighttime awakenings. It predicts sleep maintenance insomnia.
Rhonda: I have experienced...So that's one of the problems that I actually have. It's much, much better now that my stress level is, like, maintained. At graduate school, I would get nighttime awakenings where my heart would start racing. And I would wake up thinking that there was a spider or some kind of threat. And I would scream, and sometimes fly out the bed. I mean, you know, and just...it would scare my husband, you know. At the time, we weren't married. But, I mean, you know, these nighttime awakenings, it was something that's dated back for quite some time. But really, it manifested during a very stressful period, and that was graduate school.
Matt: We see that...
Rhonda: Got much better.
Matt: ...so frequently.
Rhonda: Yeah.
Matt: But if you can think about that as sort of, you know, a stress management component to insomnia, you know, it's part of what we call cognitive behavioral therapy for insomnia, which is sort of dealing with that stress, you know, meditation. There's great apps out there, like Headspace, for example.
And the data on meditation and insomnia is very very powerful. You know, I'd known about it a little bit, but I hadn't read really all of the studies until I started researching it for the book. And I was so convinced that I started meditating. And I haven't stopped since. Because it was, you know...Typically, I'm not a bad sleeper. I'm a light sleeper. I'm a pretty good sleeper. I found it hugely useful for times when I was under stress, or when I was traveling and jetlag. It's very beneficial, too.
But that underlying theme, I think, as a message for insomnia, it's not the only cause of insomnia, but it seems to be if there's one common sort of rule that binds many of the patients with insomnia together, it's this overactive fight-or-flight branch of the nervous system. And if you can settle that down, you are certainly on the path towards better sleep.
Rhonda: Right. And to kind of just...Another point that you made talking about, you know, the hormonal response and the cortisol rising typically when it's supposed to be falling, that kind of prevents you from falling asleep, there is some interesting research that I've read where, and I know you and I have talked about how the importance of bright light exposure...Bright light exposure for six hours a day...I mean, no one does that nowadays. We're always inside. So it's rare unless you're, like, working out in a nature park or something.
Matt: The irony of these things...
Rhonda: Right, you know.
Matt: Yeah. It's for the camera. I promise.
Rhonda: Right. But, actually, it was shown to lower cortisol by 25%.
Matt: Yup.
Rhonda: So this is, like, you know, another kind of I don't know if that would even help someone with the anxiety or, you know...
Matt: No, I think it's...there's no studies testing it yet, but there are studies...So just sort of to go back to make this point, we normally have a circadian rhythm, this beautiful sort of 24-hour rhythm. And we human beings were diurnal, and we like to sleep at night, be awake during the day. We have this awesome upswing of our circadian rhythm sort of once we wake up sort of 7, 8, 9, 10, 11. It starts to peak during the day. It drops down a little bit in the mid-afternoon. And that's why you sort of get around meeting tables in the middle of the afternoon these sort of, you know, head nods. It's not people listening to a good music. It's like, actually, it's a pre-programmed dip in your alertness. And then it rises back up, and then it drops down at night.
And one of the ways that you can get this sort of what you would want, which is a nice sinusoidal wave, you want a nice strong peak of the circadian rhythm during the day so that you're awake and you're active during the day and you're productive, and then you want an awesome sort of trough throughout the night so that you sleep soundly, deeply, and in a stable fashion.
And the way that you can sort of help your circadian rhythm have that wonderful peak and delightful trough is by getting lots of daylight during the day but lots of darkness during the night. And we are a dark-deprived society in this modern era. And it is a huge problem in the evening.
But I think people have underestimated that we are a light-deprived society during the day. So what happens is that your brain goes through life in this kind of almost stupor state where it's not getting enough daylight to really keep it ramped up throughout the day so you're sleepy throughout the day and you're tired, but then we've got too much light in the evening so you end up being awake at night, and then you're sleepy during the day, you're awake at night.
And so, you know, almost like, I'm gonna call it a seesaw. I think we call it teeter-totter here. You know, during the day, you want daylight to come in and force you all the way on to the on switch and you're active and awake. And then at night, you want the signal of darkness to come in to trigger the release of a hormone called melatonin to shift you all the way into the off position so you go into deep sleep and a sound sleep.
But now, with artificial light and staying out of bright light, so the teeter-totter has just pushed a little bit to one side, and then sort of with not enough darkness at night, it's only pushed a little bit down on the other side. So you kind of have this flip-flop switch that...it's like a dimmer switch that is basically just on dim for 24 hours rather than light and complete darkness, if that makes some sense.
Rhonda: Yes.
Matt: It's terrible analogy, but...
Rhonda: Do you have any idea, like, how much bright light exposure, like, you know...Let's say, you know, a lot of people work in, like, a little cubicle where they could don't even have windows. I mean, they're just like in the middle of this, like, little rooms with no actual sunlight coming in, you know, is something like if you wake up in the morning and you go outside for 30 minutes or an hour first thing in the morning, like...Most people are drinking their coffee. Well, maybe what you need is bright light exposure instead of your coffee, or drink your coffee outside.
Matt: Right, yeah. Take the coffee on...
Rhonda: Yeah. Do you know how much light you need? And if you don't have light outside, let's say you live in London, and you're in the winter, and there's no...It's just gray.
Matt: Even that, even on a cloudy day, the lux intensity of light far exceeds that that you would have from incandescent light or at sort of typical lights inside of a building.
Rhonda: Okay. So now my second question, the lux amount, so do you know?
Matt: Yeah. So I think, I mean, if you look at the studies, once you get over a sort of, you know, about 5,000 to 10,000 lux, you can have a pretty powerful effect. I don't believe there's...and I could be wrong. And Satchin Panda, our good friend, who is just A plus...In fact, yeah, if you're watching this, like, stop watching this now. Just go and watch the Satchin Panda podcast. He's much more powerful and eloquent than I am. But they have looked at the degree of exposure to outside light, not necessarily the intensity of light during that outside exposure time.
So I don't think we yet understand exactly what the dose response is in terms of lux intensity. What we do know is that getting 30 to 40 minutes of outside morning light is critical. But here's the trick. Here, in California a lot of people make this mistake, but even in London, it happens despite cloudy day, people put shades on in the morning. Don't do that. I know it looks good. But don't. Let that natural light penetrate your eye. There's a retinal mechanism that goes through to your thalamus that then goes through the hypothalamus that regulates your circadian clock. You need that light penetration. You're losing all of that good stuff if, or some of it, if you put shades on.
Wear some protection, that's fine. Just nix the shades in the morning. In the afternoon, reverse the trick. And this is actually a very good tip for jet lag. Jet lag is essentially an extreme form of what most of us have, which what we've been describing this diluted amount of light during the day and then too much light at night. Jet lag, you really should get out in the morning, 40 minutes of daylight, no shades. And in the afternoon, it's fine to go out. But when you go out, now is the time to put shades on, because you can start to encourage even then the release of melatonin, which is that hormone of darkness, which signals the timing of healthy sleep.
Rhonda: So about what time in the afternoon would you say shades are...?
Matt: So I would say, you know, probably...it depends on your bedtime, if you're a morning owl or an evening lark, and we can speak about chronotypes. So it really depends on when you're planning on going to bed. But let's say that you're planning on going to bed at about 10 p.m., I would say, if you're sort of going out after about to 4:30-ish, now is a good time to maybe start to help dilute down some of that light.
But then, you know, in the evenings, you know, we are so bathed and saturated in light. And yes, we can speak a lot about LED screens, and they are impactful, and there's been lots of work on that, some of which haven't replicated but many of which have. I think the bigger problem is just overhead lighting in general. We're just infused by, in every room that we go.
And my recommendation has now been, in the last hour before bed, just turn off half of the lights in your house, you know. We don't necessarily need all of them blazing in the last hour before bed. And when you do that, it's quite surprising how soporific and somnogenic it actually is, you know. And I want to do the experiment, although someone beat me to the experiment, and they did it...you know, it's one of those studies when I read it, I just thought, my first reaction, I'm not a big person. My first reaction was, oh, I'm so jealous.
Rhonda: Oh, yeah.
Matt: I was like, oh, I wish I've done...And then I just thought, this is a brilliant paper. I can't wait to teach it. They took a group of people. They looked at their habitual amount of sleep that they would typically get. And these people are getting sort of seven and a half to eight hours. And they would ask, you know, "When are you gointo sleep?" And sort of most of them would go to bed like 11 and sleep through till 7.
And then they took them out of that typical, you know, modernity environment, and they took them out to the Rockies. And they had sleep tracking equipment on them. They took them there for several weeks. And there was no electricity whatsoever, not even a torch, not even a headlamp from a car, nothing. And then they look to see what changed.
The first thing was that these people went from sleeping, you know, an acclaimed seven and a half or seven hours of sleep that was their norm. It was actually just below seven, saying, "That was fine. That's all I needed." To then, actually, when they had no watch, they didn't know when to wake up, no alarm clocks, they ended up sleeping closer to nine hours a night, which is what we typically see when you saturate sort of people away from or dislocate them from modernity.
Rhonda: So would you say that's a good sleep duration?
Matt: Well, I think somewhere between seven to nine is what we recommend. But I think when you do this in a healthy, young people, and these were healthy, young people, they seemed to acclimate to a sleep amount that was somewhere between sort of eight to nine hours of sleep. So I think it's good evidence that, you know...You can look at how hunter-gatherer tribes were sleeping. And we've studied, you know, these people. And they actually sleep in a strange manner. We can get back to that. And people have tried to use them as the gold standard as to how we should be sleeping.
Rhonda: They're a lot more active and...I mean, they're so different, right?
Matt: I don't think it's a good control. I think we should say, "Let's take modern human beings and let's just take them out of all context of modernity. And let's see how they're sleeping. Let's just sort of put them on an ad-lib buffet of sleep. And they can just sleep as much as they want. They're not told when to wake up and sort of when to go to bed." And they seem to sleep what we now think of as a natural amount, which is somewhere between, if you look at the distribution, seven to nine hours.
Rhonda: And these are younger individuals? Sure.
Matt: Yup. And we can speak about, and I hope we speak about sleep and aging. But what was also interesting is when they slept, not just how much they slept. They started to go to bed earlier and earlier and earlier, and they started to wake up a little bit earlier and earlier. And the total duration of sleep expended. But where that expanded amount of sleep was positioned on the 24-hour clock was dragged back because they weren't influenced by these cues of, you know, too much daylight at night. Temperature is another one that I'd love to speak about, too.
But what's fascinating is that when you look at hunter-gatherer tribes, all these experiments of sort of true nature, the natural point of middle point of sleep, the middle phase sort of time of that eight to nine hours sleep phase, came somewhere between midnight and 1:00 p.m. And I often ask people this question, you know, "Have you ever thought about what the term midnight actually means?" You know, it means the middle of the solar night, which is the time when most of us should be in the middle of our sleep phase.
But now, in the 21st century, we've gone through the, you know, the agrarian sort of, you know, pushed into the industrial era, and now into the digital era. Now midnight is the time when we maybe check Facebook for the last time or think about sending that last email. So not only has the duration of our sleep decreased through the influence of the modern times but also when we're sleeping has been dramatically shifted, too.
Rhonda: Right. I know I've made some changes a few years ago to my place, where now, I was telling you, I have Philips hue lights that turn on red light. And they come on actually quite early. They come on around 5 p.m. In fact, when we have visitors, they start to go crazy when sunset, and it's like red, and they're like getting sleepy, you know. It's like, "Why is it so dark in here? Can we turn the lights on?" And it's like, "No, because that's what you should...You're supposed to be getting the sleepy right now. You're supposed to be...It's 6:00, 6:30." Well, depending on what time of year it is, you know, "The sun is setting. You should be getting sleepy." It's phenomenal.
Matt: Yeah. It's one of the few triggers.
Rhonda: Yeah, it really works.
Matt: Temperature is the other key trigger that...I think that's probably, you know, in the past three years, that's what we've really understood, is that temperature is as powerful a trigger of sleep organization and sleep depth as light is.
Rhonda: And sleep depth.
Matt: And sleep depth as well. So what typically happens is that, for you to fall asleep and stay asleep, your body needs to drop its core temperature by about 1 degree Celsius or about sort of 2 to 3 degrees Fahrenheit. And that's the reason that you will always find it easier to fall asleep in a room that's too cold than too hot, because the room that's too cold is at least taking you in the right thermal direction for good sleep. It's dragging your body down into a cooler realm.
And when you look at these hunter-gatherer tribes, you know, the San in Namibia, you can look at them, whose way of life hasn't changed for thousands of years, they don't go to bed and necessarily as immediately as the sun goes down. They usually go to bed maybe sort of 8 or 9 in the evening, several hours after sundown.
But when they do start to go to bed is when the temperature drops. As the sun drops, the ambient temperature remains for a little while, and then it starts to drop, too, as the land cools, and the ambient temperature cools with the land because darkness has ensued. That seems to be a thermal trigger for them getting sleepy and falling asleep.
Then, when you look at when they wake up, they typically wake up 15 to 20 minutes before dawn. So it's not light that seems to be necessarily the trigger instigating the awakening. It's actually the rise of temperature.
Rhonda: And that's on a circadian rhythm, right?
Matt: And that's on a circadian...So what is training us to our natural sleep rhythms is both temperature and light. So this comes back to our modern homes, where we go into offices, and we don't necessarily have the rising warmth of the day to activate us because we're set at 70 degrees, and then we go home, and our thermostats are set at 70 degrees again or whatever your standard temperature is. And we don't get the thermal cue through our bodies to say, "It's time for sleep." So no wonder our sleep is worse.
And if you manipulate people's core temperature, and you can do this through showers, hot baths, you can do it through saunas, but there's a great experiment where they essentially designed what it looked like a kind of a wetsuit. And throughout the wetsuit were all of these plastic veins running through them. And the researchers were able to exquisitely control, through water at different temperatures, the temperature of any part of your body. So would I want to warm your hands and your feet? Or would I want to warm your core?
And so what they were able to do is...These people I mean talk about being stripped of your dignity, you know. You get into this like wetsuit, you zip it up, and you say, "Right, I'm off to bed." In you go. And then they would manipulate core body temperature exquisitely. And lo and behold, when they dropped the core body temperature, they were able to induce sleep quicker, and the amount of deep sleep, what we call slow-wave sleep, which is deep non-REM sleep or Stages 3 & 4, also called slow-wave sleep because of these big powerful slow brainwaves, that deep, rich non-REM sleep was increased somewhere between about 10% to 20%, which is non-trivial.
Rhonda: Wow.
Matt: Then they said, "Well," this is in sort of, you know, young healthy people, "what about people with insomnia, and people who are older." Because older people struggle with sleep and, of course, insomnia. And they were able to get even greater of mileage out of the thermal manipulation with those cohorts, too. So I think it's a very interesting intervention possibility to try and augment and manipulate human sleep.
Rhonda: So do you think those things, like the chili pads that are out there, you think those can potentially help deep sleep?
Matt: Yeah. I don't know of any data from them yet. All I know is the experimental data that we've looked at, you know, with manipulation of body temperature. They did this in rats awhile back, by the way, which is they would warm their paws. And when they warm their paws, the rats fell asleep quicker and stayed asleep.
And you think, hang on a second, you just told me that you need to cool the body, but you're talking about warming them up. And this is the reason why probably saunas work, hot baths work, and showers work for the opposite reason that most people believe them to work. You think, you know, I get out of a hot bath, and I'm nice and toasty, I get into bed, and I fall asleep faster.
That's not true. What happens is that you get into the bath, you get massive vasodilation. All of the vessels open up on the surface of your skin. That draws, it almost charms, the blood out from the core of your body to the surface. And your skin and your hands and your feet especially act like these wonderful thermal radiators. And they dissipate the heat. So you get out of the bath, and your core body temperature actually plummets, and that's what you need for good sleep.
And I suspect this the reason that saunas...I mean, I think you've had experience it too.
Rhonda: Yeah, definitely. It definitely affects my sleep. And going from a sauna into, like, an ice cold shower and then doing kind of like going back and forth really really helps sleep. And I've used that also going to other countries. Getting in the sauna and going the cold shower and then back in the sauna.
Matt: And triggering it back.
Rhonda: It helps with my jet lag.
Matt: Yeah.
Rhonda: I mean, it's an end of too, because my husband experience the same thing. But, you know, there's definitely something...there's something there. And what you're saying absolutely happens. The sauna increases vasodilation, blood flow goes to the skin, and so dissipation of heat. That all makes perfect sense. So hot bath...
Matt: I'm just gonna, very quickly, just grab a quick mouthful of water.
Rhonda: The hot baths and hot showers are good before bed.
Matt: Yeah. And I'll just mention, I think one thing that's I think fascinated me, though, about the benefit of exercise...so exercise also has a really nice, powerful benefit on sleep, although it's a two-way street, and remind me to talk about that, in a good way. But something else has occurred to me with saunas, too. And I was thinking about this, because I think I know that you're a fan. I think you've mentioned this before. One of the ways that you can induce sleep is that you can increase a lot of the immune factors, things like cytokines, you know, things also like TNF-alpha, or...
Rhonda: IL-6.
Matt: IL-6. IL-1 even more so, but IL-6 is part of that equation, too. We've known this for some time that if you infect an animal, it will create an immune antibody response, a cytokine cascade. Those cytokines have a direct communication pathway into brain structures, including things like the hypothalamus, which regulates sleep. And it's that immune cascade that is actually a trigger in dialing up the amount of sleep. So when animals get sick, just like when humans get sick, the thing that you want to do is just curl up in bed and go to sleep.
And in fact, you get sleepier as a consequence of being infected. Why is that? The reason is because there is nothing better...Sleep is the Swiss Army knife of health, that no matter what the ailment...
Rhonda: That's so cool. I don't know...
Matt: You know, there is something more than likely in the armament of sleep toolbox, sort of as it were, that will deal with that, and so, and I promise I'm not going off on a tangent here, so the idea is that these immune factors are sleep-instigating.
Rhonda: This is awesome. Wow.
Matt: They are sleep, sort of, you know, they're somnogenic, you know. Somno-sleep, genic-increased genesis, improvement. So what I've been thinking about is whether or not the sauna, the benefit of the sauna, is both thermal, but is also, by way of this powerful immune pathway...
Rhonda: It does.
Matt: ...that you get this.
Rhonda: That's phenomenal.
Matt: And I've read some of the studies, and I'm blanking on his name, you will probably remember his name, they've looked at some of essentially sort of, you know, the sauna-induced immune responses.
Rhonda: Yeah, so that Charles Raison has been doing that work.
Matt: Thank you. Yeah.
Rhonda: Yes.
Matt: Thank you. Brilliant. Yeah, so I've read some of Charles's papers.
Rhonda: Yeah, we had him on the podcast. He was talking about how the sauna induces IL-6 and some of that stuff. And the same thing that happens with exercise. So that's...
Matt: Yes. So that's why I mentioned exercise, which is that I think...
Rhonda: Wow, that's so fascinating.
Matt: So now we're all starting to sort of, you know, realize how the sleep system is augmented, one of those paths, you know, is light. The other is darkness. The other is temperature. But here's a fourth one. The immune system. And we know that you can inject, you know, some of these cytokines into animals, and you can almost induce sleep. It's that powerful.
Rhonda: That's so cool.
Matt: So now I'm starting to think, I wonder if some of the sauna-based benefits and some of the exercise benefits, because when you exercise, you also typically get some of these pro-inflammatory cytokines that sort of get released to perhaps deal with some of, you know, the essential distress. And, you know, I think we've both spoken about this that...
Rhonda: So that way, like if you're exercising a lot, you do seem to require more sleep, or you sleep more?
Matt: Well, we don't know that, but that's my current theory...
Rhonda: Yeah, it's a great hypothesis.
Matt: ...which is that, you know, you possibly...
Rhonda: Are you gonna test that? That's awesome.
Matt: Yeah, we're going to test. So we've just actually been looking at studying not with exercise or with saunas but we've had been looking at sleep and pain. And when you deprive people of sleep, you get a chronic release of these pro-inflammatory cytokines, which is not a good situation. Acute, great, somnogenic, good for the body. But chronic long-term, we're starting to piece together a brain-body-sleep-pain interaction, which I think has, we haven't published this yet, but should have marked implications for the hospital environment. Because the one place where you do not get a good night of sleep, where it's architected against the night of sleep, is the one place where you need sleep the most, and it's usually the one place where you are in pain the most.
And I want a revolution to happen regarding sleep in hospitals. And I'm desperately trying to work with folks. For example, the NHS in the United Kingdom, National Healthcare System there. I would love to work with any hospital system in the U.S. to solve this crisis, I think, of sleep in the hospital environment.
But, to come back to your point, this is a great experiment to do. You know, is exercise-induced acute inflammation, and is sort of, you know, heat/shock sensitive, you know, induction of immune responses by way of saunas or hot baths, are those a pathway triggering good sleep? And if so, can we find novel therapeutics for, you know...
Rhonda: I'll put you in touch with Dr. Jari Laukkanen too. He's in Finland.
Matt: Okay.
Rhonda: He's, like, the leading researcher on saunas and...
Matt: Has he done some of the stuff on longevity?
Rhonda: He's the guy doing all the longevity, Alzheimer's disease, cardiovascular disease...
Matt: Yes, yeah, yeah. I've read some of his work. Yeah, yeah, yeah.
Rhonda: Yeah, I mean, and he's a friend of mine as well. So I'll put you in touch with him.
Matt: Okay.
Rhonda: Because that would be really cool if you guys could...
Matt: If we can start tracking their sleep, you know, and see perhaps. And you can sort of put this into a statistical sort of triangulation, which is called the mediation analysis. And you could see, you know, what's causing that longevity benefit. Because we know for example that the shorter your sleep the shorter your life, that short sleep predicts all-cause mortality. It's also probably one of the most significant lifestyle factors determining whether or not you'll develop Alzheimer's disease. And all of these things I know have been linked to, for example, sauna, which is longevity, decreased susceptibility to the development of dementia and cognitive decline, is part of that...I'm not trying to say it's all about sleep. But, the part of it about sleep, you know...
Rhonda: Really, you know, one of my major interests is aging, increasing healthspan, as well as performance, without the trade-off, and every time I always come back to sleep. The studies, I mean, it just constantly coming back in my face how important sleep is for all those things.
Matt: It's the superordinate lever that transacts all health benefits, you know. It's the tide that rises all of the health boats. And I think it's wonderful that folks, you know, here in Silicon Valley are going after, you know, individual pathways of disease, trying to manipulate, you know, immune pathways or trying to manipulate mTOR for sort of, you know, longevity.
But I think what's been missing in this equation is that there is, you know, an Archimedes lever here. There is one superordinate node, that if you pull that lever, all of the other pathways are instigated, activated. And that superordinate node or lever is this thing called sleep. You know, there is no physiological system that we've been able to measure that isn't wonderfully enhanced by sleep when you get it or demonstrably impaired when you don't get enough.
Rhonda: Right. I kind of wanted to go back, because you were talking about the effects on how the immune system can be, you know...what did you call it? I mean, it induces sleep.
Matt: Somnogenic.
Rhonda: Somnogenic, yes. How it's somnogenic. So interesting. I had no idea that the cytokines were responsible for that, and it makes perfect sense. So, anyway. But also, so the opposite is true where sleep also affects the immune system, or a lack of sleep also, right?
Matt: It does, yeah.
Rhonda: And that is something, you know...Your immune system is the first line of defense against, even pretty much everything, right: cancer, viruses, bacteria.
Matt: Yeah.
Rhonda: And I think in your book, you were talking about the effects on, some studies, on natural killer T cells. I mean, I was just, like, blown away by some of the numbers.
Matt: This is a frightening study. So it's done by my colleague Mike Erwin. You take a group of individuals, and you're not going to deprive them of sleep for an entire night. You're simply going to limit them, restrict them to four hours of sleep for one single night. And then we're going to measure the amount of reduction in natural killer cell activity.
So just to take a step back, natural killer cells are a critical part of your immune defense arsenal. And today, both you and I and everyone listening to this podcast, we all have cancer cells that have emerged in our bodies. But typically, what prevents those cells from becoming this disease that we call cancer is, in part, these natural killer cells. So what you wish for is a virile set of these sort of immune assassins, these sort of James-Bond-like, you know, that they will annihilate these foreign organisms. You want a virile set of those at all times.
So take a group of healthy people, limit them to four hours of sleep for one night, and what you see is a 70% reduction in natural killer cell activity, seven zero. That is an alarming state of immune-deficiency. And it happens quickly essentially after one bad night of sleep. So you can imagine, you know, the state of your immune system after weeks, if not years, of insufficient sleep. And it's now the reason I think that we probably are finding, at the epidemiological level, significant links between short sleep duration, not getting enough sleep, defined as six hours or less, and your risk for the development of numerous forms of cancer. Currently, that list includes cancer of the bowel, cancer of the prostate, cancer of the breast.
And the link between the lack of sleep and cancer is now so strong that, recently, the World Health Organization decided to classify any form of nighttime shift work as a probable carcinogen. So in other words jobs, that could induce cancer because of a disruption of your sleep-wake rhythms.
So, you know, that's the immune system in cancer. But it doesn't stop there as well. Another great study that was done by Eric Prather [SP], who is over at UCSF, another good colleague of mine, he did this brilliant study that I write about in the book. He basically measured the sleep of a group of healthy people for a week before using these wristwatches that are accurate. And then he quarantined them in a hotel, in a set of hotel rooms. And then he proceeded to stuff up their nose, squirt up their nose, rhinovirus, essentially, a flu virus. And then he quarantined them for a week. And he measured how many of them became infected. And he was measuring all sorts of stuff. He collected every ounce of snot that they blew out of their nose, all of the mucus, everything.
And what he found was that those people who were getting five hours of sleep or less in the week before they came in and were infected relative to those who are getting seven hours of sleep or more, those people who were getting five hours of sleep in the week before they got infected were four times more likely to end up developing the flu than those people who are getting seven hours or more.
The final nail in that sort of immune coffin for me is a study that was done by Eve Van Cauter, who's a wonderful endocrinologist. And I'd love, by the way, to speak about sleeping diabetes and glucose regulation, too. She's doing some great work there. But she did a great study. She looked at the amount of sleep that you were getting in the week before you get your flu shot.
And what she found is that if you're getting sort of less than five or six hours of sleep in the week before you get your flu shot, you only produce half of the normal antibody response, rendering that flu shot largely useless, which stuns me that, you know...And here's where technology could revolutionize healthcare. You know, what if Kaiser, you know, had access to a sleep tracker or had its own sleep tracker. And Kaiser, for those not familiar, is a health care provider here in the United States.
But what if, you know, any healthcare provider or system in any country had access to your sleep in a non-Big-Brother way. And it was tracking your sleep. And through an app, it would say, "Hey, you've had a great week of sleep this weekend in December," or "this week in November. Now is the time to come and get your flu shot. I've listed out three appointments. Just tap on the one that you want."
Or it says, "Look, I know that you scheduled yourself for a flu shot. You haven't quite got the good sleep that you need this past week. Let's try again next week." And if you get the sleep next week, then you give them access to getting the flu shot. Because otherwise, we're wasting money. And the flu, you know, cost the United States, the flu season cost the United States about $10 billion directly in terms of healthcare burden. Even if I could nudge that by just 1% or 2% by understanding people's sleep and helping architect a system that co-opts around sleep time and management, we could save hundreds of millions of dollars to the U.S. economy.
Rhonda: Wow. Speaking of the flu, I think I even told you this in a previous conversation, like, I almost never get sick. Maybe once a year, I'll get a little runny nose for a couple of days. I've got a really good immune system generally speaking. But this last year, I had a baby, and along with having a baby comes sleep deprivation. And there's absolutely nothing I can do about it. I mean, you have to wake up multiple times to feed your baby. And so that's what I was doing.
And, I mean, I got the flu. I got a cold. I mean, I was sick, like, every month. I mean, it was crazy. I've never experienced...of course, my baby luckily was getting all my antibodies and didn't get sick, thankfully. But it was, like, completely connected to my sleep.
Matt: It's impressive, isn't'?
Rhonda: Yeah. I mean...
Matt: It's the same wisdom that, you know, mothers would sort of say, you know, that speech. You're getting sick a lot. Are you sleeping enough? You know, and I've often thought that people like me, sleep scientists, all I'm really doing is putting the data behind everything that your mother and Shakespeare ever told you about sleep. You know, I'm just putting data. They have knew it all long before the data came along. But you see that exact same thing in parents. Sickness is rife in those early years. You see it in medical resident.
I think a friend of yours, who I enjoy this, too, a lot, Peter Attia, was saying this about when he was in medical residency, and you see this in residence, too, you know, sickness rates, you know, increased dramatically. There is weight gain, the diabetic profile, you know, in terms of their ability to manage glucose becomes markedly impaired. We know that testosterone in men plummets when sleep gets short. In fact, men, who are sleeping five hours or less will have a level of testosterone which is that of someone 10 years their senior.
Rhonda: Wow.
Matt: Which, in other words, a lack of sleep will age men by a decade in terms of that aspect of virility and wellness.
Rhonda: How quickly does that happen? Do you know? Is that like...?
Matt: So you can see that within almost days once you start to dose people on that. It comes about quite rapidly. You can see hormonal change. I mean, I think that's what...if there is a major access...oh, sorry, axis within the body that is altered by sleep it is the hormonal axis. I think that principally, through the root of the autonomic nervous system, that is the lens through which almost all sleep and sleep deprivation effects can be viewed.
And I'm just starting to write up a theory paper about this, which is an encompassing theory about sleep deprivation within the human brain and the body. And I think there is a common, central dictating governing pathway, which is the autonomic nervous system through which there is a manipulation of many of the hormone systems, which then give rise to the whole host of deficits that we see by way of a lack of sleep, which then ultimately, through chronic exposure of sleep loss, give rise to all of the diseases that we know are associated with a lack of sleep. And every single disease that is killing us in the developed world has causal and significant links to a lack of sleep.
Rhonda: One that I'm particularly interested in is Alzheimer's disease. It's something that I've been researching for a while. I'm about to get published thankfully soon.
Matt: Congratulations.
Rhonda: Thank you.
Matt: Was this a review paper?
Rhonda: Yeah.
Matt: Oh, please send it to me.
Rhonda: And it happens to do with a gene called APOE4. And I found out that I have one copy of this of this allele. And when I found that out years ago, I was like...it's probably the biggest risk factor for late-onset Alzheimer's disease besides age.
Matt: Yes. So I think one of those alleles, it's about sorts of two to threefold risk.
Rhonda: Two to threefold.
Matt: If you have two of them, it's like an 8 to 12.
Rhonda: Yeah, it's, like, pretty bad. And 25% of the population in the United States has at least one allele. So it's definitely...And just because you have it doesn't mean you're necessarily gonna get Alzheimer's disease.
Matt: That's right.
Rhonda: Not everyone has it. But there's a huge interaction with, you know, diet and lifestyle. Probably the biggest lifestyle interaction with this gene is sleep. And so that was that was where I became very interested in how sleep affects the brain, and how it affects, you know, Alzheimer's disease, and all that. So I'd love to kind of talk a little bit about that.
Matt: Yeah, so we've been doing a lot of this work. We have a large research program here at UC Berkeley at the Sleep Center that is devoted to aging and Alzheimer's disease. And we've been very fortunate to get many grants from the NIH here to study this. I think that the story is fascinating because it's a bi-directional relationship between sleep and the pathology that we know is associated with Alzheimer's disease.
So in Alzheimer's disease, there are at least two protein culprits that we believe are underlying of the brain pathology that seems to create this thing called Alzheimer's. One of them is a sticky toxic protein called beta amyloid that accumulates in these clumps outside of brain cells. And that creates these amyloid plaques that seem to be correlated with your disease risk and disease severity.
The other is a protein that we know probably less about, which is a protein called tau protein. And that sits inside of cells. And it creates a support structure for communicating and funneling many of the critical ingredients up and down your nerve cells to keep them in rude health. And during Alzheimer's disease, that protein starts to sort of fall apart and dismantle. And you get these sort of tau tangles. And the structure of the nerve cell and its ability to transport all of the ingredients that it needs to operate starts to collapse and fails like a tunnel collapsing down.
So one of the discoveries that we made back in 2013 was that I was looking at the distribution of this sticky toxic protein called amyloid in the human brain. And what's fascinating is that it doesn't build up in the brain homogeneously. Amyloid builds up in some parts of the brain far more severely and early in the course of Alzheimer's disease. And other parts actually remain completely uninvaded by this thing called amyloid. In fact, parts of the motor cortex, for example, or parts of the visual cortex, you see almost no amyloid in our Alzheimer's patients. And that's probably the reason why their motor functions and their vision is unchanged.
But one of the earliest places where beta amyloid builds up and then built up most severely in late stages is back, again, in that medial prefrontal cortex that sits right there in between the eyes. Why was I interested in that? I was interested because when we were doing studies where we would map, with all of these electrodes over your head, we would map the deep sleep that you were having.
And we could do some clever mathematical modeling of those deep sleep brain waves. And we could try to triangulate where was the electrical epicenter of those electrical deep brain waves of deep sleep. And it seems as though they come from all over the brain, but the principal epicenter that generates your deep sleep sits right there in the middle part of the prefrontal cortex. It is exactly the same part of the brain that accumulates toxic beta amyloid protein.
Then we've done studies, and other people have done studies before us, that demonstrated, as we age, our sleep gets worse. But not just any type of sleep. Especially that deep quality of sleep that we know and we spoke about is critical for saving and learning and retaining new memories. So all of these jigsaw pieces started to get put together in my head. I thought we need to do some studies. Is it possible that the amount of amyloid that you have in the brain in this sleep-generating center, it should directly predict the deficit in the amount of deep sleep that you get? If it predicts the deficit in the amount of deep sleep, it should predict the deficit in your ability to hold on and retain new memories, which is a hallmark cognitive feature of Alzheimer's disease, difficulty learning, difficulty retaining.
So we did the study, and it's exactly what we found. The more beta amyloid that builds up in this central frontal part of the brain, the less the deep sleep that you have. The less amyloid-related deep sleep that you had, the more forgetful you were the next day rather than the more that you remembered. So this was the first part of the Alzheimer's sleep equation, which is that Alzheimer's disease attacks the deep-sleep-generating regions and you have a diminution of deep sleep, which, in turn, blunts your learning and memory abilities and you become more forgetful.
A far more important discovery was made by an another group, far more important than the one we made, which was essentially the reverse direction, which was to say, "Rather than amyloid sort of decreasing sleep, could sleep actually decrease the amount of amyloid that you get?"
And this is a discovery that was made in rats back in 2009, I believe, was the first evidence that was published in science. A colleague, [inaudible 01:24:09], who is out on the east coast at the University of Rochester, and she made two wonderful discoveries. The first was that we've known for a long time the body has a waste sewage system called the lymphatic system. But the brain doesn't have its own lymphatic system. The lymphatic system does not penetrate the brain. So where does all of the garbage, the metabolic garbage go that your brain cells produce? Where is the sewage system for the brain?
And she discovered it. It's actually made up of a set of cells called glial cells, which are these supporting brain cells. And so she called it the glymphatic system rather than the lymphatic system. So your brain does have its sewage system, this glymphatic system, and that's the discovery that she made. Remarkable.
Then, and I'm not quite sure what motivated her to do this, she started to measure how efficient that glymphatic, that waste system was when the rats were awake and when the rats were asleep. And what she found was that it's during deep sleep that these brain cells actually shrink by almost 60% when we sleep. Blows my mind.
Rhonda: Yeah.
Matt: It's almost like, you know, all of the buildings in New York all of a sudden shrink, and it leaves these much greater, large areas for the cleaning crews to come in and clean up all of the metabolic detritus of the city's activity during the day. It's exactly what happens during sleep. And the cleaning solution is what we call cerebrospinal fluid. And through a pulsatile mechanism during sleep, you get a 10% to 20% increase in the bathing of cerebrospinal fluid through the brain, which washes away all of the metabolic byproducts that have been building up. One of those metabolic byproducts is beta amyloid. And, in fact, if you deprive those rats of that deep sleep, you immediately get an increase in toxic beta amyloid.
So now we've linked these two. I'm sorry it's a long story. But if you're not getting enough deep sleep at night, you're not giving yourself the chance for the kind of good night and sleep clean process to remove the beta amyloid. So more beta amyloid builds up. Where does it build up? Tragically, in the very same regions of the brain that generate the deep sleep that you need to clear out the toxic amyloid. So you start getting less deep sleep, so you get more toxic protein, more toxic protein, less deep sleep, less deep sleep. It's a self-fulfilling prophecy, and it's a nonlinear exponential curve.
If you look at how amyloid builds up in the brain, and if you look at the trajectory of Alzheimer's disease, it is a nonlinear exponential curve. It fits exactly what the sleep-dependent model of amyloid clearance would predict. If you're not getting sufficient sleep, that's the reason why now insufficient sleep seems to be one of the most significant lifestyle factors determining that.
Now you could say, by the way, those studies were in rats, and you deprived from the sleep for one night. What about humans? Like, surely...Well, the study has now been done. Great study done out of Wash U by a team of scientists led by David Holtzman. And they took a group of humans, and they did this very clever method where they deprive them of deep sleep but they didn't deprive them of sleep.
And you think, it sounds paradoxical. I can play you these auditory tones. Now this is not like the memory reactivation where you play a tone and then you leave the brain alone for a while. Here, I'm just going to keep playing tones to your brain, really sort of annoying tones. But I can play them at a level that doesn't wake you up, but it lifts you out of deep sleep and keeps you in shallow sleep.
So what's delightful about this method is that I can selectively excise one type of sleep, deep sleep, but I don't wake you up. So there's no stress of awakening. You are asleep for the same amount of time, but the quality of sleep is decreased.
Rhonda: Can street noise do that?
Matt: We don't know. Although I will come back to that when we speak about hopefully sleep appetite regulation, sleep glucose regulation, and sleep in low socio-economic cultures...
Rhonda: This is a little terrifying.
Matt: And I think that it's possible. I think there's other factors that link poor sleep in low SES, socioeconomic backgrounds. Is noise pollution one of them? I actually think it is. Untested as yet. But what they did with these human participants, they selectively remove deep sleep while keeping them asleep so total sleep time has not changed. And then, in the morning, they woke them up, they rolled them over, and they did a spinal cord puncture, a lumbar puncture, and they measured the cerebrospinal fluid that was percolating within the spinal cord, which also goes around the brain. And you can measure the amount of beta amyloid, which is a reflection of perhaps how much amyloid is there within the brain.
After one night of essentially a loss of deep sleep, you saw an immediate rise in the amount of beta amyloid. So it is a causal manipulation. That insufficient sleep in rodents and in humans will lead to a rise in beta amyloid.
Rhonda: Yeah. I think it was like 25% to 30%.
Matt: It was.
Rhonda: Yeah, it was definitely...So, of course, that's all I could think about the past nine months...
Matt: Showing that, yeah.
Rhonda: And the buildup of amyloid.
Matt: You know, I would tell you, that's the last thing you should think about. You know, try not to worry too much about it, you know, because it's not to say to diminish the loss of sleep but simply to say that worrying about it is not gonna do you any good.
Rhonda: Of course.
Matt: But how do you tell that especially to people who, you know, have one ApoE allele...apoe-4, sorry, allele. What I would also say that's important for people, if you know your ApoE status, and if you are apoe-4, be mindful of snoring as well. Because people who are apoe-4-positive, they also have a significantly elevated risk of a sleep disorder that we call sleep apnea, which is sleep disordered breathing, which is heavy snoring and a cessation of breathing entirely. And then you gasp when you wake up again.
Heavy snoring sleep apnea is a killer. It is an outright killer. It increases your risk of basically everything you don't want: cardiovascular disease, stroke, diabetes, and obesity. It also increases your risk of immediate death through a higher risk of car accidents.
But one of the other problems with sleep apnea is that you don't get the amount of deep sleep that you need. And you have hypoxic damage. Because you stopped breathing, your oxygen saturation goes down. You get hypoxia damage particularly in a region that is most sensitive to it in the brain, which is, drumroll, the hippocampus, the very same memory structure that is attacked in Alzheimer's disease.
So now you can see why I appeal for this sensitivity in this danger to sleep apnea. Because if you are apoe-4, you're already at high risk of Alzheimer's disease, you need to pay attention to your sleep. If you start snoring, and you have sleep apnea untreated, you will get less deep sleep. So you're compromising the thing that you need to try and lower your amyloid risk to begin with, because you're going to build up that amyloid, because you're not going to get the amyloid clearance elsewhere in the body, for example, in the liver. And then worse still, the part of the brain that is attacked severely by Alzheimer's disease and atrophies, which is the hippocampus, which is why memory fades, is a part of the brain that is damaged when you stop breathing because of oxygen desaturation.
So, as an appeal, even if you are not apoe-4-positive, but you are snoring, or you know someone who is snoring, go and see your doctor and get a sleep apnea test. It is potentially life-saving.
Rhonda: Actually, I had a sleep apnea test because of my night awakenings. I didn't know. It was, like, maybe I have apnea and I couldn't...And so I'm having this terror. And of course, that wasn't it. I don't have sleep apnea. But I didn't know about the connection between apoe-4 and sleep apnea. That's terrible because...
Matt: It's quite a dramatic...
Rhonda: Yeah.
Matt: I mean, you combine those two together. It's a real...I mean, it’s gasoline on an already started fire.
Rhonda: People with apoe-4 also don't repair damage and their brain as well as people with apoe-3.
Matt: They don't.
Rhonda: So you're talking about hypoxic damage in addition, you know, there's sort of just this potentially compounding effect.
Matt: And I think that's, you know, that's part of the reason...I mean, so I have some family members that have been associated with Alzheimer's disease, one recently passed away. And it's been a big motivation for me personally. I started, you know, 20 years ago. My PhD was looking at people with degenerative dementia. That's how I actually got into sleep, because I was seeing these sleep abnormalities.
And, you know, I'm so desperately trying to find ways to help and to combat that incredible epidemic of dementia. And that's why we've started to try and develop things like electrical brain stimulation methods, to try and help actually augment human sleep, an electrically-supercharged sleep, as it were, to see if we could give back some healthy quality of deep sleep to patients who are aging or those with dementia. Can we essentially, you know, amplify the amount of deep sleep? And in doing so, can we salvage aspects of learning and memory? But better still, could we actually start to increase, you know, the amount of glymphatic clearance of beta amyloid?
Now I suspect that when the disease is in play and you've been diagnosed in those late stages, I don't know how much sleep is electrically charged even as it may be could help. What we're now trying to do in our studies is actually retrospectively find out, is there a particular decade of life or decades of life when a decline in sleep makes you most susceptible to then developing a lot more amyloid later in life? In other words, we're trying to now identify these vulnerability windows during the lifespan.
The reason I want to do that is, if I can scientifically convince myself of a knowledge base of vulnerability sensitivity to insufficient sleep, my guess is that it's just across the lifespan, it gives me a chance to know where is the inflection point of not late-stage life treatment but early-life prevention. Because that's what medicine has to do right now, I think. We've done a good job at extending lifespan but a miserable job at extending healthspan. Lifespan is probably about treatment. Healthspan is probably about prevention.
Sleep needs to be part of that discussion. And sleep is usually absent in many of these conversations for either lifespan or healthspan despite it having a demonstrable impact on both. But my hope is that to be able to find that sensitive time when your risk for Alzheimer's development by way of insufficient sleep is present. That's where I go in and start augmenting your sleep with electrical brain stimulation or other methods that we're trying to develop as well.
Rhonda: I think, at least for the APOE-4-positive individuals, by the age of 40, the amyloid plaques start to really...
Matt: That's right, yup.
Rhonda: ...you know. So, to me, it would seem that, you know, before 40, and certainly, when you hit 40, you better have your sleep optimized.
Matt: I would say before. I mean, we can see the decline of deep sleep occurring in people in their 20s. That's when your deep sleep starts to decline.
Rhonda: Wow.
Matt: Which is, you know, frightening, isn't it? It's sad. And at that point, it's in the mail. You know, by the time you're 50 years old, you've lost about 50% of the deep sleep that you are having when you are a young teenager. By the time you're 70%, there's only about 5%...sorry, by the time you're 70 years old, there's only about 5% of your deep sleep left that you had when you were young and healthy. By the time you're 80, we almost can't detect any of these deep sleep brain waves anymore.
Rhonda: Do you know if there is changes in the way your core body temperature regulates with age as well?
Matt: There is. So what happens with age is that your circadian rhythm that we've spoke about before...I'm just going to...So your circadian rhythm that we spoke about before, which in healthy people is nice and high and peaking during the day, lots of activity, and then drops down at night, lots of inactivity, lots of deep sleep, that sinusoidal wave starts to flatten out as if someone has compressed it as we get older. So our circadian rhythm gets weaker. So we get we feel sleepier during the day and not as alert as we used to do, but we don't feel as though we are as sleepy at night. We're more awake at night because our circadian rhythm is blunted.
And so I think that's another area for aging intervention, is how can we modulate the circadian rhythm. And it turns out that it comes back to light. So one of my colleagues in the Netherlands, Eus Van Someren, did a great study where he installed circadian-regulating light in an elderly care home, you know, in a home where you care for the elderly. And many of them had cognitive decline. And he's now done some of these studies with people in with Alzheimer's disease in some of these care homes.
And when you start to create appropriate lighting in the internal environment in these homes, which if you go into them, and I used to go into them all the time during my PhD, these sort of care homes, and I would be testing my patients and seeing my patients there, they were grim environments with dim light. And these patients never got outside. They rarely had a window. And Eus Van Someren, the scientist in the Netherlands, he was able to really produce this strong bout of light during the day inside the care home and then drop out that light in the evening. And he regularized their light. And he improved the circadian rhythm. And he improved cognitive outcome measures.
Rhonda: Wow.
Matt: Cognition got better in these Alzheimer's patients.
Rhonda: That's cool.
Matt: Now you can look at that same manipulation, that same lighting hack, at the beginning of life. So in the neonatal intensive care unit, what we used to have when we'd go in there, you just have constant light on all of the time, dim light on 24 hours a day, which prevented those infants getting the signal of a regulating 24-hour light-dark cycle.
If you regularized light in the neonatal intensive care unit, so light during the day, darkness at night, in these studies, what you see is basically almost a 50% to 60% increase in oxygen saturation within the blood of these neonates in the intensive care unit. Weight gain increases dramatically. And they end up exiting the neonatal intensive care unit at about five weeks earlier than they would otherwise.
Circadian regulation of sleep leads to better health outcomes. It does so in neonates. It does so in the elderly. So I think there is all manner of sleep possible interventions that we can think about across the lifespan when it comes to modifying disease risk at any stage of life.
Rhonda: Yeah. And I think, at least as far as I've, you know, understood from our conversation thus far, some of the main things for prevention in optimizing your sleep really are preventing that emotional stimulation, that anxiety, and getting particularly a few hours before bed, the bright LED exposure early in the morning, and then not having the bright light exposure, you know, about four hours before bedtime. And then the cold, like, having your body temperature go down. So, you know, whether that's through something like, you know, having a hot bath or a hot shower or even possibly the chili pad, which I'm gonna actually experiment with...
Matt: Yeah.
Rhonda: Because now I've been using this Oura ring that I've been tracking my sleep. By the way, do you know how accurate, like...So it tells me, in my app, the light sleep, the REM sleep, and deep sleep. And I know there's nothing going in my brain measuring any sort of brainwaves. So it must be movement, right, that...
Matt: Yeah, I won't say specifically even though I know the folks at Oura and I know the folks at almost all of the sleep-tracking companies, most of them right now use a combination of your heart rate, which you can pick up through the pulse waveform either on the wrist or on the finger, or if it's a bed sensor, through the heartbeat, as well as respiration. And they'll use a combination of those things together with movement to try and stage your sleep.
Right now, without naming, you know, I don't think there's anyone that is necessarily better than the other, at least none of them have published scientific evidence. We sleep scientists have actually looked at these devices relative to gold standard, what we call polysomnography, which is essentially like doing a sleep study. If you were to, here at my sleep center, we've got all of this equipment. You look like a spaghetti monster with electrodes on your head.
Rhonda: I don't know who can sleep with that on.
Matt: Yeah, I know. But we can measure that sleep with high precision, high fidelity. That's the gold standard. And when you compare these sleep trackers, unfortunately, they're not quite accurate. They either overestimate or underestimate sleep onset latency, how long it takes you to fall asleep. They either overestimate or underestimate the amount of time that you've been awake. Sleep duration may not be bad with some of them, total sleep duration, but once you get into the sleep stages, that's where things become more inaccurate. Their ability to separate non-REM from REM, it is getting better. It could be in the region of sort of 60% accuracy, possibly lower. But right now, we're not there yet. Will we be there in about four years' time? I actually think we will be.
Rhonda: Because that's what...I'm really interested in the deep. Obviously...
Matt: But also I would say REM sleep, too, you know, I think REM sleep takes a backseat. At sort of, you know, a bit of a neglected stepsister in the sort of sleep conversation. REM sleep, we found all manner of different functions, one of which is emotional first-aid. It's incredible for palliative emotional benefit. It's not time that heals all wounds, but it's time during REM sleep that provides emotional convalescence.
Rhonda: I guess that would also then be important to help you sleep better, because if you are managing your emotions better, you probably have less anxiety...
Matt: Correct. Exactly. But also REM is for the body, too, you know. It seems to regulate cardiovascular function. So REM sleep is critical too.
Rhonda: Oh, really? Is REM what's important for lowering the blood pressure?
Matt: No. Well, it's during deep sleep that you get this lowering of blood pressure, and we've got some data right now that we're about to publish that deep sleep provides actually a homeostatic recalibration of blood pressure.
What do I mean by that? If I measure your blood pressure before sleep and then after sleep at a matched circadian time, so we remove the circadian fluctuation of which there is a large one to your systolic blood pressure, but we match it, and so the only thing that's different is the quality of your sleep, what we've discovered firstly is that the amount of deep sleep that you have measured in these big delta slow waves during deep non-REM sleep, that predicts how much of a drop in your systolic blood pressure you will have in the morning relative to the evening as if deep sleep provides a recalibration of the cardiovascular system.
Rhonda: Wow.
Matt: If you're having higher frequency brainwaves that are not like the deep sleep, that's what we call unrestorative sleep, if you have a ratio of very little deep brainwave activity and a lot of high-frequency wake-like brain activity, what we call delta-beta ratio, that predicts very bad cardiovascular outcomes, that if anything, your systolic blood pressure is even worse after sleep than it is the night before.
And what we found is that during aging, now we looked at this and healthy people, then we replicated in older adults, and we found that the older that you get, the less deep sleep that you get, the more sort of wake-like or faster-frequency brainwave activity, which isn't good during deep sleep. And that accurately predicts the cardiovascular dysfunction that we see in aging. So we now think we understand in part why poor sleep is linked into poor cardiovascular outcomes.
One of the benefits of sleep is that it resets cardiovascular tone and particularly systolic tone. It doesn't stop there. There's lots of other benefits, heart rate drops, etc. But REM sleep also seems to have this strange function where you go through these cycles where you get a massive activation of the cardiovascular system, and then it falls silent, and then a massive escalation again. And you get this really remarkable increase in heart rate variability.
And heart rate variability has been used as a metric of health outcome, that if you have high heart rate variability, it's very good. It predicts lots of health outcomes. That's what you get during REM sleep. So we should be careful not to think of everything being all about deep sleep. It's about all stages. Every stage of sleep that we have, we have ascribed a function to. Which makes sense, you know, during sleep...Sleep is the most idiotic of all things in terms of a creation from Mother Nature. You know, you're not finding a mate. You're not reproducing. You're not eating. You're not caring for your young. And worse of all, you're vulnerable to predation. So on any one of those grounds, sleep should have been strongly selected against in the course of evolution.
The exact opposite is true. Every species that we've studied to date sleeps. What that means is that sleeper has fought its way through heroically every step along the evolutionary pathway, which must mean that if sleep doesn't serve an absolutely vital function, it is the biggest mistake that the evolutionary process has ever made. And if any one of those stages of sleep could be removed, because it was not important, because I want to, you know, emphasize this type of sleep because that other sleep must not be important, I promise you, mother nature would have thought, I'm gonna excise that stage of sleep out because you're just too vulnerable.
But I think, in your position, of course I would be concerned about my deep sleep, thinking about things like APOE-4, Alzheimer's risk, too. But I think the bottom line is that no matter which way you slice the sleep pie, you just can't shortchange sleep.
Rhonda: I just want to figure out, it'd be nice to know what environmental factors are affecting, you know, different stages of sleep, you know. So it's like, you know, if I do X, then that's gonna, you know, affect my deep sleep or it's gonna affect my REM or it's gonna make me miss, you know.
For example, if I were to go to bed, let's say I usually go to bed at 9 or 9:30, and if I were to go to bed instead at 11:30 or midnight, because I had a social event or something, and my circadian rhythm, usually, well, my circadian rhythm these days is my son. Wakes me up at 6 a.m. But let's just say I could sleep longer if I...let's say I wake up at 6 a.m., but then I'm like, "Oh, I went to bed at midnight instead of 9:30. I'll try to go back to sleep." Would that be okay? Would I be able to, like, recover something that I'm missing from the 9:30 to midnight? Do you see what I'm saying? Like...
Matt: Yeah. So...
Rhonda: Should I go back to sleep? Should I try to go back or...?
Matt: You should try to go back to sleep. So you should try to get the sleep that you need.
Rhonda: The duration, yeah.
Matt: Yeah, the duration. So there are essentially four ingredients, and this is probably going to be my next book, which is essentially the four pillars of sleep: depth, duration, continuity, regularity. If you shortchange sleep on any one of those, you get a compromised deficit in brain and body. So depth is what we were speaking about. It really should be depth/quality of sleep. You need both the depth of those deep sleep brainwaves but you also need all of these different brainwave oscillations, these things called sleep spindles, and slow waves, and the coordination between those two. It's all about the electrical quality of your sleep.
So you can have the duration of sleep, you can have eight hours of sleep, but if it's not of the right electrical quality or depth, you get deficits. But you can get lots of high quality sleep, but if you're only getting four hours of it, it's not going to be enough. So it's duration. Depth, duration.
Then it's also about continuity. This has been probably, in the past five years, one of the explosions in the sleep field. If you were to get eight hours of sleep but across a nine-hour period because you are awake for, you know, 5 minutes here, 10 minutes here, 30 minutes here, 15 minutes here, that's very fragmented sleep, which, by the way, alcohol is another thing that will fragment your sleep very much like that. So the continuity of your sleep is poor. It's not continuous. It's fragmented.
And even if you get eight hours of sleep in a nine-hour period but it's fragmented versus you get eight hours of sleep all in a nice one bout within eight hours, so in both of those scenarios, it's the same duration of sleep, maybe it's even the same electrical quality of sleep, but if it's fragmented and littered and punctured with many awakenings, the continuity of sleep is poor. And that's not good either.
And then, finally, the part is regularity. This means going to bed and waking up at the same time no matter whether it's the weekend or the weekday. Go to bed at the same time, wake up at the same time. Those are the four key pillars that we know of for sleep. And you can hold any three constant and manipulate one of them and you get a deficit.
Now we can't quite weigh the complete, you know, is it, you know, this one is worth, you know, 40%. This one is worth sort of 20%. We can't yet do that. But it's very clear that those are the four pillars of good sleep.
So I mentioned that just coming back to the quality of sleep, when you position the quantity of sleep on the clock face, on the 24-hour clock face, at an inappropriate time according to your natural innate preference, and I say that specifically rather than a particular time, you will not get the same quality of your sleep. So an extreme version of this is a night shift worker, where they may get eight hours of sleep in bed but they are sleeping during the day, not during the night. So it's a complete reversal. The quality of their sleep is not good. They don't get the same amount of deep sleep nor do they get the same amount of REM sleep.
But let's kind of walk that back a little bit to your scenario, which is much more subtle. Let's say that my chronotype, and your chronotype simply determines whether you're a morning person, an evening person, or somewhere in the middle, about 30% of the population is an extreme morning type or a morning type, about sort of 40% percent is sort of neither strongly morning or evening, and about the remaining 30% is an evening type, we call them owls and larks.
So if you're a morning type, you like to go to bed, let's say, like, 9 p.m. And wake up at 5 or 6. If you're an evening type, you may want to go to bed at 1 a.m. And wake up at 9 a.m. The next morning. So when I'm saying the optimal position of sleep, I'm saying with the optimal for your chronotype, this is your chronotype...And by the way, it's genetic. You don't get to decide whether you're a morning type or an evening type. It's hardwired into your genes. We know the genes. It's not your fault. If you're an evening type and you're listening to this, and society, which is strongly architected against your chronotype, we reward and we favor the morning types, it is not your fault. It's not a choice. And there's not too much you can do about it. You can push and pull the system by about 30 minutes, 45 minutes, but not much more.
So coming back to it, when we position that sleep on that eight-hour period, whatever is optimal for you, you will get a nice distribution. You'll get all of the deep sleep that you want and all of the REM sleep that you want. And earlier in the conversation, I said that we go through these 90-minute cycles, we, human beings, it's different for different animals, you always go into deep non-REM sleep first and then you always have REM sleep second. And that repeats every 90 minutes throughout the night.
What changes, however, is the ratio of non-REM to REM within those 90-minute cycles as you move across the night such that in the first half of the night, the majority of those 90-minute cycles are comprised of lots of deep non-REM sleep and very little REM sleep. In the second half of the night, that balance shifts, and now you get much more REM sleep in the late morning hours and very little deep sleep.
The reason I'm saying this is because let's take someone who goes to bed at a substandard amount of time. Let's say that they go to bed at midnight, and they're going to wake up at 8. But instead they have to wake up, because they've got an early morning meeting, so they go to bed at midnight and they wake up at 6. And my question is how much sleep have they lost? And your response is, well, they've lost two hours out of the eight hours, which means they've lost 25% of their sleep. And your answer would be right in a way, but it would be wrong as well, which is that they've lost 25% of their total sleep but they may have lost almost 80% of their REM sleep because that's the REM rich phase of the night.
And it also works the other way around, too, that if you go to bed too late, you will...So what happens is, because of the circadian rhythm, the brain has a different appetite for different stages of sleep on the 24-hour clock face. In the late evening and the early morning hours, the brain has a dietary preference for deep sleep. And it doesn't very much have an appetite taste for REM sleep. Through to the second half of the night, that's when it gets its appetite for REM sleep.
So if you start sleeping at 4:00 in the morning and you wake up it in the middle of the day, your brain has lost its appetite for deep sleep. And so it won't get much. Now you will probably get much more REM sleep as a consequence. So you've got to be really careful. That why...
Rhonda: So it's almost like your chronotype may even dictate in a way how much deep sleep you may get.
Matt: The chronotype will...If you sleep naturally and you get the amount of sleep that you want, your chronotype will probably mean that...your circadian rhythm is actually shifted as your chronotype, too. So you will still get, as an owl, if you get your eight hours when you want it, you will probably get a similar sleep architecture as a lark, who has gone to bed five or six hours earlier, because your circadian rhythms are five to six hours different.
But you're right in the sense that owls typically try to go to bed early. But because they are designed not to fall asleep at that time, they're just gonna lie in bed. Many owls think that they have insomnia. They don't. They're just not going to bed at the right time. Because they get into bed, and it's like a teenager, whose rhythm is also shifted late, you tell them to go to bed because you've got to wake up for early school start times, but there's nothing they can do because their circadian rhythm has shifted forward in time. And it's the same for owls.
So what will happen is that they will probably stay awake for a while, then they'll get into deep sleep. But then they have to wake up at an earlier time, and they will lose a lot of REM sleep. REM sleep, for emotional well-being, what the owls typically experience: depression, low mood, anxiety. So I think we're really starting to put the pieces together on that component.
Rhonda: And so for someone like me, I'm somewhere in the middle, like, when I don't...pre-baby. Now I'm I guess you would call a lark because I'm going to bed at, like, 9. My optimal time, if I can go to bed when my son does, and it's like, you know, if I go to bed, like, at 8, then I get the longer duration. That way, if I'm a little more fragmented, then I, like, at least can make up for it somewhat. But I'm up at 6 a.m. Now if it were up to me, I'd like to sleep...I usually would wake up, like, 8 a.m.
Matt: Yes, 8 a.m.
Rhonda: Like, that's my natural time.
Matt: And the reason that you can probably go to sleep sort of, you know, 9 p.m. Or even 8 p.m. Now is because you're chronically sleep-deprived. And as a consequence, you've built up such as sleep debt that, you know, there is a lingering what we call sleep pressure in your system. But, yeah, I think fighting your chronotype, we found, it comes with deleterious health consequences. Increased risk for poor cardio-metabolic outcomes. Things like, you know, C-reactive protein is higher. If you look at, you know, A1C in terms of sort of a Rorschach review of blood glucose, your blood sugar, not good. If you look at your propensity for being obese or being overweight, also not great if you're an owl and you're not sleeping according to your schedule.
Rhonda: Telomeres are shorter.
Matt: Telomeres are shorter as well.
Rhonda: So let's talk about your, because a lot of interesting research has come out of your lab on the blood glucose regulation front and, well, I guess more on the eating preferences...
Matt: And appetite and eating.
Rhonda: ...and appetite. Yeah.
Matt: I mean, the way I see it, it's all part of the energy intake expenditure system. And sleep, you know, if you think about like a weighing scale between sort of energy expenditure and energy consumption, sleep, if you're not getting it, just annihilates that balance. And we can speak about any one of those things.
But, you know, I think the blood glucose story and sleep is very very well-worked out now. It started with epidemiological studies, where we started to see that people who were sleeping less than seven hours were at significantly higher likelihood of either being diabetic or going on to develop diabetes. Many of them were already, you know, what we call a pre-diabetic state, or they had what we now call sort of metabolic disorder.
And then the question became, well, is that associational or is it causal? So the next studies that happened in this was work back in...starts in the 1990s by Eve Van Carter at the University of Chicago. Wonderful studies. It took a group of healthy people, started to limit them to different doses of sleep for a week, you know, five hours of sleep, six hours of sleep, four hours of sleep, and what she showed was that, essentially, after one week of short sleep, your blood sugar levels are disrupted so significantly that your doctor would classify you at that point as being pre-diabetic after one week of short sleep.
And the way that they do this is what's called a glucose tolerance test, where you are fasted, and then you are given this sickly-sweet drink of glucose, and then they are measuring from your blood in the next three or four hours how quickly is your body able to dispose of that blood glucose.
So what happens when you drink or when you eat a meal is that your blood sugar spikes. And you don't want that spike to stick around very long. If your body is healthy, it deals with that raised level of blood glucose very quickly, and it brings it back down very quickly. That's a healthy profile. That's what we call good glucose management. So how good is your body at disposing essentially of that glucose? And the way it disposes it is that cells in the body, including muscle cells, will suck up that glucose. And it's called your disposal index, or your disposition index, it turns out.
So what she found, Eve Van Carter, with her studies, was that, firstly, the way that your body knows how to absorb glucose and suck in that glucose is that there is another chemical called insulin, which is released by the pancreas, beta cells of the pancreas, and that insulin will instruct the cells of the body to open up special glucose channels to absorb the glucose and your blood sugar drops, which is good and healthy.
Firstly, what she found was that when you are not getting sufficient sleep, the beta cells in your pancreas stop being sensitive to the signal of high glucose. So the beta cells, which normally are listening for this spike in glucose, and as soon as they sort of, you know, hear...no, they're not hearing it. They're sensing it. But as soon as they sense the spike in glucose, they release insulin. And that insulin will drop your blood glucose.
But those cells had become insensitive to glucose, what we call sort of glucose insensitivity. And so the beta cells of the pancreas stopped releasing as much insulin. It didn't release enough insulin to drop blood glucose, so blood glucose remained high. If that wasn't bad enough, we've since gone on to demonstrate, and you can do this with really clever studies, taking tissue biopsies, the cells of the body including muscle cells and fat cells, their receptors stopped being as sensitive to insulin.
So, firstly, you're releasing less insulin when you're sleep-deprived. But what little insulin you do release is not instructing those cells to open up the channels to take away the monsoon of the glucose that's flowing in the channels of the body. So on both sides of the glucose regulation, on the release of insulin, to instruct cells to absorb glucose, and on those cells themselves to be sort of instructed by insulin, those cells became less sensitive to the insulin signal. And so, as a consequence, your overall ability to deal with glucose became far more degraded, and blood glucose remained higher, which sets you on a profile of looking pre-diabetic.
Rhonda: Couple that with the standard American diet, and, you know...
Matt: And you're off to the races in terms with...
Rhonda: Yeah, and eating late at night. So, actually, are you familiar with the studies, I know Dr. Satchin Panda actually is the one who told me about this, melatonin is actually what is responsible for shutting down the pancreatic beta islet cells from producing insulin. So I wonder how much of the sleep deprivation the melatonin system is involved in that.
Matt: Yeah. So in those studies, what was good is that they held constant circadian rhythms, they held constant ambient light, and they even held constant physical activity. The control group was sort of they were in bed for eight hours, but the people who are sleep deprived, limited to four or five hours, during the eight-hour window where the other people were actually sleeping, they had to lie recumbent in bed with no physical movement.
Rhonda: Oh, man.
Matt: So you controlled, but it was a great study because you control for physical activity as well. So we now really understand the link between a lack of sleep and poor glucose management, and very very well indeed. And we also know the stage of sleep that's important. It's, again, deep slow-wave sleep. The study that I described before, where you're playing those annoying tones just below the level of awakening so I can remove your deep quality of sleep, you can do that same thing again, and you essentially produce that same diabetic-like consequence just by removing or excising deep slow-wave sleep.
Rhonda: So you're doing that, and then on top of that, some of your work has shown that you're now also gonna have a preference to eat the very food that raises your blood sugar, right?
Matt: Yup, yup.
Rhonda: And it's something I've definitely experienced...
Matt: High glycemic food...
Rhonda: Yeah, yeah.
Matt: So this is a whole...So it all fits in, I think, to this energy balance. So, you know, firstly, what we know is that your regulation of blood sugar, of blood glucose is profoundly impaired by a lack of sleep. But what about your calorie intake? What about your obesogenic profile, setting aside your glycemic profile?
So what we've discovered is that when you're not getting enough sleep, two appetite-regulating hormones go in opposite directions. These two hormones are called leptin and ghrelin. And I often, you know, think of them as, you know, they sound like hobbits to me, at least, you know.
Rhonda: That's hilarious.
Matt: Leptin and ghrelin that, you know, J. R. Tolkien would have written about them. But they're not. They're real hormones. Leptin is a hormone that signals satiety. What I mean by that is, when you have high amounts of leptin, it tells your brain you're full. You're satisfied with your food. You don't want to eat anymore. Ghrelin is the other hunger hormone. When ghrelin is increased, you feel unsatisfied by your food. You feel hungry. And you want to eat more.
So after you eat a meal, normally, what happens is that levels of leptin increase and levels of ghrelin, the hunger hormone, you can think about ghrelin as like a grumbling tummy, ghrelin goes down. And this means that you stop eating, you don't want to eat anymore, and you're full for a duration of time period. When you are sleep-deprived, levels of leptin, which normally signal to your brain you're full and you're satisfied with food, that hormone is impaired by a lack of sleep. So you lose the fullness satiety signal in your brain.
If that wasn't bad enough, the hunger hormone, ghrelin, actually increases. So it's a double whammy effect here. What does that lead to? It leads to a strong obesogenic profile of energy consumption, of food consumption. So what we, and Eve Van Carter, in fact, has done all of these pioneering studies, and we've done some of them now, too, typically, you tend to overeat during main meals. So you will typically eat somewhere between about 200 to 300 extra calories. If we give you a meal, and we measure all of the food on your plate, and we ask how much did you eat at that one sitting, you tend to overeat by about 200 or 300 calories per main meal sitting.
Rhonda: Wow.
Matt: Now you could say...Well, actually...
Rhonda: That's after a full night of sleep?
Matt: Well, that's when you've been limited to maybe four hours of sleep for a week. Now someone, and the reviewers of these papers, you know, in the early days, said, "Well, that's because when you're awake longer, being awake is more metabolically demanding, and you're probably moving around more." Not true. It turns out sleep, firstly, is a remarkably metabolically active state. You're very active metabolically when you're asleep. In fact, the difference between being asleep versus being awake is only about, for a whole night of sleep, the difference of about 140 calories.
Rhonda: Wow.
Matt: Just like a small cookie, essentially. So, yes, when you're awake longer, you do burn more calories. But the amount of calories that you increase in your intake far exceeds anything that you expend by way of being awake a little bit longer. If that wasn't bad enough, though, it's not the main meal where the trouble lies with sleep. That's some of the problem.
The other studies that are even more sort of devilish are where you give these sleep-deprived subjects the same meal but then you give them a snack bar. And it's an ad-lib food buffet, essentially. And you can eat as much as you want. And they allow you to eat in a room by yourself, so there's no social pressure, so you don't restrict your eating or...it's true eating.
And of course, we measure everything that you eat. And it's snacking that is the dead giveaway here. You end up eating 300 to 400 additional calories by way of snacks. This is after they've eaten a 2,000-calorie meal in one sitting. They will then go away, and they will eat an additional 400 calories at the snack bar.
Rhonda: Wow.
Matt: So, as a consequence, what you're doing is you're increasing the total caloric intake, which sets you on a path towards being overweight and obese. Then the discovery came that it's not just what you eat...sorry, it's not just how much you eat but it's what you eat. And what Eve Van Carter discovered in her early studies was that if you give one of these sort of food buffets...and you can eat anything. It goes from, you know, sugary treats to salty treats like pretzels or potato chips to heavy-hitting starchy carbohydrates, breads, pasta, pizza all the way to salad, what you find is that you eat more of all of the food groups. But you eat mostly in terms of an increase the starchy, heavy-hitting carbohydrates as well as the sugary foods.
And if we know anything from the recent movement in food, particularly from people like Gary Taubes, who has written wonderfully about this type of stuff, that's the food that sets you on a path, again, down an obesogenic and also a poor glycemic control profile. If you look at all of the cardiometabolic markers of health when you're eating excessive carbohydrate-heavy rich or and particularly simplified sugars, they're bad for your health profile in general. It's exactly the foods that you eat when you are underslept.
Rhonda: Is there a feedback loop on those foods affecting your sleep?
Matt: There is.
Rhonda: There is.
Matt: So I would say this is probably, apart from maybe the gut microbiome of which there is now some evidence, and we're starting to look at this, too, at the sleep center, it's probably the least well understood. But the bottom line is that if you're eating a diet that's high in carbohydrate, especially high in processed simple sugars and low in fiber, you tend to have worse sleep, you take longer time to fall asleep, the amount of deep sleep that you get is less, and you have more fragmented awakenings throughout the night.
Now I don't think there's enough evidence right now for me to hang my hat on any dietary prescription for sleep. In five years' time, I think we'll have a very different conversation. I think, you know, absence of evidence is not evidence of absence. I think we'll get there. And I think food is going to be a big part of that equation. I think we have gut microbiome, too. I think that's what we've seen when you, in a few of the studies where you limit people, you sleep deprive them or you put them on a jet lag routine, you see the balance between the sort of bacteriodetes sort of class of the microbiome versus the firmicutes. That ratio goes in a balance that you don't want.
So, typically, in sort of obese people or people with diabetes, you get a higher ratio of the firmicutes relative to the bacteriodetes. When you modulate sleep and you shortchange sleep or you put sleep on a jet like profile, that's exactly the same gut microbiome sort of dysregulation profile that you see. So I think it's gonna be a great...And I think part of...
Rhonda: Because they're on their own circadian rhythm as well, the...
Matt: They are. Yeah.
Rhonda: So is that why? Because their ratio is changing and then...?
Matt: I think it's possible that it could be a circadian rhythm. I think it's also possible that it could be down to what we described before, which is the fight-or-flight branch of the nervous system, that when you are under slept, it's, like, revving a car but in neutral. It's desperately bad for the engine. That's what happens when you're sleep-deprived. You get this ramping up of your fight-or-flight system, and it just stays there with chronic sleep deprivation for as long as you're chronically sleep-deprived. And one out of every two adults in first world nations is chronically sleep-deprived.
I think it leads to a release of stress chemistry, particularly cortisol. Cortisol is known in the gut microbiome to produce this imbalance. What's the pathway? I think it's probably a bunch of nerve fibers from the brain into the body called the vagus nerve. And we're starting to do a lot of work on this now. I think the vagus nerve we know has a direct mainline pathway or provides a mainline pathway from your brain to your gut. And that's why there is a very powerful brain-gut relationship.
I think that's one of the mechanisms by which the gut is affected by sleep. Which gets me excited, because if that's true, flip the equation, could the gut microbiome be a path through which we can reverse-engineer a signal for better sleep in the brain? I think that now becomes a parsimonious hypothesis, and it's one that I'd like to test as well.
Rhonda: There was a really interesting study looking at the effects of a particular strain. I think it was the rhamnosus strain that...they produce GABA in the gut.
Matt: Yes.
Rhonda: But GABA doesn't cross the blood-brain barrier as far as...I think most evidence suggests it does not.
Matt: No. So the brain has GABA, but it's not coming from the...
Rhonda: Right, right.
Matt: Yeah.
Rhonda: But there was some studies that were speculating that there's, through the vagal nerve, because some of the efferent neurons in the gut were stimulating it, and they were more, like, relaxed or something. They were producing GABA in the brain through the vagal nerve. And GABA affects sleep, right?
Matt: Yeah.
Rhonda: So it sounds like there could definitely be some sort of interesting...
Matt: You know, that's one of...I think the things in anxiety that we see is that it's a failure of the brain to dampen down and basically invoke inhibition throughout the brain to quiet down these regions.
Rhonda: That particular strain of probiotics was shown to help with anxiety. Small trials, clinical trials in humans. Of course, the initial studies were preclinical in animals, but it has been shown to actually help improve...
Matt: It does?
Rhonda: Yeah. [inaudible 02:14:04]...
Matt: My guess is that, if that's true, if you were to look at sleep, I would be surprised not to see a sleep benefit by way of an anxiety reduction. I think, I mean, in my lab, that's probably one of the most reliable things that we see when we deprive people of sleep, of any dose.
Rhonda: That anxiety goes up?
Matt: Anxiety goes up. We've done the dose response curve. We've looked, you know, hour by hour by hour. And as soon as you get past probably about 14 or 15 hours of wakefulness, anxiety starts to increase. The further you go into that sleep deprivation period, the more anxious that you get. It's a very robust, reliable effect.
Rhonda: So what do you think...It sounds like if you were to give people, like, some of the main things, you know, the main interventions they can do to help improve their sleep, a lot of people are interested in prevention, a lot of people listening and watching are really interested, including myself, in prevention. And it sounds like things that lower anxiety are obviously important for...
Matt: Critical.
Rhonda: Yeah, for improving sleep.
Matt: Yeah. I think the prescription I would have...Well, firstly, I think it's good to recognize the sort of those four pillars of sleep that, you know, depth, duration, continuity, regularity, but I think there are five actionable things that people could do tonight to start getting better sleep. And we've mentioned many of them. The first is darkness. You really do need some degree of darkness at night to release that hormone melatonin, which helps trigger the timing of the healthy onset of sleep.
Rhonda: And you would say about maybe four hours before your bedtime, or what would you say...?
Matt: Yeah, I would say three to four hours is the time to start thinking about your light saturation exposure, certainly in the last hour before bed. And there are ways that you can do that you can install software on your computer if you really have to look at it, but I would advise against that because I think computers cause and trigger anxiety. I think, in fact, if anything, my estimation right now is that the blue light from those screens is detrimental. I think the evidence is favoring a blockade of melatonin and a reduction in REM sleep.
They did this great study. They took people with an iPad, one hour of iPad reading versus one hour of book reading. iPad reading dropped or blunted melatonin by over 20%. The peak of melatonin didn't arrive until three hours later. This is one hour of iPad reading. They had less REM sleep, and they...
Rhonda: They were reading, like...?
Matt: They were reading just a book under dim light versus reading the same book on an iPad. When they woke up the next morning, the people who read the iPad felt more unrefreshed. They subjectively knew that they had not slept as well. What was interesting is that when they stopped the iPad reading, there was a washout effect that was a blast radius of reading the iPad. And it's continued into subsequent nights even though they'd stopped reading the iPad.
So I think light is a feature, but I also think part of the problem with computers and iPads and iPhones...and I don't mean to sound like a prude about this, but they do trigger anxiety. They are what I would describe as anxiogenic pieces of hardware. Unless you are, and if you can do this, please write to me and tell me how you do this, but most people get a lot of their anxiety infusion in part through these devices.
A recent study in teenagers are actually demonstrated that part of the reason that they were having sleep disruption by using phones was not necessarily about the light but was because of FOMO, fear of missing out, that if you weren't online, you would miss out on some key social communication. And they were suffering because of that, too.
But I digress. My first recommendation is watch the light saturation, watch the light pollution. And you can think about it like that in the evening. So an hour before bed, certainly, close computers down, try not to stare at phones, and dim half the lights down in the house. It really is powerful.
The second is temperature. Try to set your bedroom temperature to somewhere between about 63 to 66 degrees for most people is optimal, colder than most people think.
Rhonda: Yeah, that is definitely colder than...
Matt: Yeah. And if you get cold feet, it's okay to wear socks, but cold it must be. The third thing is what I would suggest is walk it out, which is don't stay in bed awake. This is one of the mistakes that a lot of people make. In this era, I think most people, because of anxiety, we're wired and tired. And one of the problems when you are lying in bed awake for a period of time, and I think more than 20 minutes is not great, because what happens is that your brain very quickly starts to learn the association between being in bed is about being awake rather than your bed being the place of sleep. And so it learns this association.
And so many of the patients that I speak to, they'll say, "Look, you know, I'm falling asleep on the couch watching television, and then I get into bed and I'm wide awake, and I don't know why." And the answer is because you've made the association between your bed is the place of wakefulness, not your place of sleep. So the answer is you need to break that association. Get out of bed, go to another room, in dim light, just read a book, no computers, and only return to bed when you feel very sleepy.
And the first night this may mean that you're awake for two or three hours. And it sounds bad, and it sounds strange coming from someone like me, but that's better than staying in bed awake for those two or three hours. And over time, gradually, by only returning bed when you're sleepy, your brain will relearn the association that it once had when you're a child, and you can relearn it, which is that your bed is a place of deep sleep and sound sleep. So that's the next thing.
I think the final two things we've touched upon a little bit, which is alcohol and caffeine. Caffeine, many people know, keeps them awake. It's a stimulant. It's what we call psychoactive stimulant. It's the only psychoactive stimulant, by the way, that we readily give to our children in an unregularized free way, which I think is a problem. Caffeine has several problems with it. Firstly, because of it being a stimulant, it can keep you awake and it makes it harder for you to fall asleep.
A lot of people, though, will say to me, "Look, I'm one of those people who can have a cup of coffee with dinner and I fall asleep and I stay asleep, and I'm just fine." Even if that's true, we and others have done these studies, if you give someone a standard dose of one cup of coffee in the evening, 200 milligrams of caffeine, the amount of deep sleep that they have is reduced by 20%. You would normally have to age an individual by 10 or 15 years to drop your deep sleep quality by 20%, or you can do it simply by having a cup of caffeinated drink or coffee in the evening. So caffeine is a problem.
The other problem with caffeine is its duration of action. Caffeine has a half-life of about six or seven hours. And a half-life simply means the amount of time it takes for 50% of the drug to still be in your system or 50% of it to be cleared. Caffeine has a quarter life of about 12 hours. In other words, if you have a cup of coffee at noon, a quarter of that caffeine is still circulating in your brain at midnight.
So if you have a cup of coffee at noon, it's the equivalent of getting into bed at midnight. And just before you turn out the lights, you swig a quarter of a cup of Starbucks, and you hope for a good night of sleep, you know, it's probably not gonna happen.
So the advice would be try to cut caffeine off around about midday if you can. And even if you're someone who, you know, can fall asleep fine, stay asleep, you should just know that caffeine can still impact your sleep.
It's what usually creates the vicious cycle, by the way, that those people will wake up the next day, they feel unrefreshed and unrestored by their sleep, they don't remember waking up, so they don't think it's the cup of coffee, but now they start reaching for two cups of coffee in the morning rather than one. They've got now more caffeine in the system. The next night, they have even less deep sleep. The next morning, they wake up even less refreshed. And now they drink more caffeine. Self-fulfilling prophecy.
Final one is alcohol. Alcohol is probably the most misunderstood sleep aid or sleep drug. It's what most people usually reach for when over-the-counter medications have failed. Alcohol is a sedative. It's a class of drugs that we call the sedatives. And sedation is not sleep. So when you drink alcohol, what you're doing is sedating your cortex. You're just knocking yourself out. And that's why you think that you fall asleep faster.
There are two other problems with alcohol. Firstly, alcohol will litter your sleep with many more awakenings throughout the night. And in fact, some people can even see this on their sleep trackers even though they're not necessarily as accurate as my sleep laboratory would be. Even with that less accurate measure, you can still see the impact of alcohol in sleep. So it litters your sleep with awakenings, fragmenting your sleep. So this comes back to the third of the four pillars of good sleep, which is continuity. It takes away your continuous asleep, and it makes it fragmented.
The final part of alcohol is that it's one of the best chemicals that we know for suppressing REM sleep alongside marijuana. Now, by the way, I should say that's THC-specific. If you look at CBD, the evidence seems to be less clear. CBD actually doesn't seem to be as detrimental to your sleep as THC. If anything...
Rhonda: Yeah, because a lot of people, I mean, again, this is just anecdotal, talk about how marijuana improves their sleep.
Matt: Yes, yeah. So marijuana...We have two separate sort of the active from the inactive component. THC, tetrahydrocannabinol, is the active component. And CBD is the sort of the non-hallucinogenic component of that.
Rhonda: They're both in if people are taking a whole plant here.
Matt: Typically, yeah. Yeah, exactly. Now with strains and drops that you can buy, you can separate those out, you can play around with the ratios, and you can get very low THC to very high CBD. THC does tend to decrease the time it takes you to fall asleep, but it tends to make you sometimes wake up more throughout the night, but it certainly does seem to block REM sleep.
One of the other problems with THC dosing of sleep is that you become dependent on that for sleep. And when you stop using THC for sleep, you have quite bad rebound insomnia, which leads to then a perpetuating cycle of dependency. And I think, you know, I'm never keen for dependency on anything, be it dependency on, you know, any, you know, food substance or anything. I think you should, you know, be able to generate all of the physiological pathways and processes that you need, you know, naturally without dependency.
CBD is interesting, though. There is nowhere near enough data for someone like me to make any recommendation. So all I can do is tell you the very limited data that there is right now. CBD does not seem to produce the degree of REM sleep impairment that we've seen with THC. What's interesting is that low-dose CBD actually seems to be wake-promoting. So you actually are sort of forcing yourself more awake. High-dose CBD seems to help people sleep more consistently.
I would have thought it would it be the opposite, that low-dose would have been better than high-dose, but the opposite seems to be true. Now we don't know about the dependency. We don't know about the long-term effects. So I am not going to sit here and give any recommendations regarding THC use or CBD use. If you're using any compound, be it alcohol, be it a sleeping pill, which are...sleeping pills, by the way, come with deathly consequences and higher risk of cancer. Or you're using...
Rhonda: Really?
Matt: Yeah, markedly increased risk.
Rhonda: Is that because there's something directly the sleeping pills are doing, or because the way it affects your...? What does it do to your sleep, sleeping pills? A lot of people take Ambien.
Matt: So in the past month, 10 million Americans have swallowed some kind of sleeping aid, either a prescription or over-the-counter, monumental amounts. You know, I often joke that I think, it's not really a joking topic, but, you know, it took George Lucas about 40 years to amass $4 billion in profit from the Star Wars franchise. It took Ambien less than 20 months to amass $4 billion in profit. That tells me everything about the insufficiency of sleep and the desperate need for sleep in this modern 21st-century era.
But the problem is Ambien isn't part of that same class of drugs that alcohol is. It's what we call a sedative hypnotic. It works on the same receptor, which is the GABA receptor. Now it tickles the GABA receptor in a different way to that which alcohol does. But what we found is that sleeping pills, and I won't name any names but including the one that you described, they are sedating the brain. You're not going into naturalistic sleep. If I look at the electrical signature of your sleep when you're on a sleeping pill versus natural sleep, it's not the same.
Secondly, what we found is that those sleeping pills can often come with a grogginess in the morning and some forgetfulness. Third, what we've found is that in animal models, and this is work that was done by Markus Frank, who's a wonderful friend and colleague, he was looking at how the brain rewires itself during sleep. And the brain does, particularly during the development.
And he has a model in animals, where, if you sort of put a patch on one of the eyes when the visual cortex is developing, the visual cortex shifts over to developing more wiring to the eye that remains open. And it's called the monocular deprivation paradigm of brain plasticity, and it's a very well worked out model of brain plasticity. If you give those animals some exposure once you patch the eye to the eye that remains, you drive learning and plasticity, and then you allow it to sleep, sleep will strengthen the synaptic connections that have been made during the day by about 100%.
Rhonda: Wow.
Matt: So sleep is almost as powerful as experience during the day. That's how sort of strong and powerful it is. But what he then did was a study where he dosed those animals with Ambien. Now it turns out that those animals slept even longer, if you look at the data, than the animals who weren't dosed on Ambien. And the prediction would be, surely, they would have as much if not more of that wonderful brain plasticity. The opposite was true. Ambien-induced sleep resulted in a 50% unwiring of the connections that have been made during day rather than potentiating them.
That frightens me. Because if you look at the prescription age of sleeping medications over the past decade, it's coming down and down. I don't know how long it's going to be before prescription medication comes in to a pediatric realm. And if those data hold up, it makes me worried. So I'm coming off topic a little bit, but we know that sleeping pills are associated with a markedly higher risk of death, as well as cancer, as well as your susceptibility to infection, particularly in pneumonia.
But returning to alcohol, it is definitely one of the most, I think, misunderstood drugs. But what I was saying regarding THC, alcohol, sleeping pills, if you are using anything to help you sleep, I think you have to ask yourself, are you just really treating, you know, an open wound and not really actually trying to stitch it up? Because what that is simply doing is masking a problem that you're not dealing with, you know. Why is it, like...?
And this is not a criticism, I'm sorry if my voice sounds like that, and it's not, you know, I'm so sympathetic to people who have sleep problems. We see them all of the time here. But you have to ask why. Why is it that you're struggling with sleep? Is it because you're of a certain chronotype and you don't understand your chronotype and you're sleeping at the wrong phase of the 24-hour period and it's masquerading as insomnia. Or do you have too much anxiety in your life and you're blunting that anxiety with things like alcohol or THC or sleeping pills? You know, you're just kicking the can down the road. You're just hitting the mute button. But the movie is still playing of damage. Whatever is causing that sleep disruption, you know, is still there. You're just sedating your brain and trying to mask it.
So I think people who are using those things, if they're having sleep difficulties, you should ask yourself, could I examine my life and really think more about what it is that is preventing me from sleeping. What's good is that you don't have to turn to any of those because there is a non-pharmacological treatment but is just as effective as sleeping pills in the short-term. It is completely safe. And it is more efficacious in the long-term. And it's called cognitive behavioral therapy for insomnia or CBTI.
Based on its efficacious nature, and they've been done lots of randomized clinical control trials, it is just as powerful as sleeping pills in the short-term. But when you stop working with your therapist, and you work with a therapist for several sessions across several weeks, when you stop working with a therapist, you don't go back to the bad sleep that you have. You continue on with your good sleep. Unlike sleeping pills, which is when you stop them, you have what we call rebound insomnia, which is that you tend to go back to the bad sleep that you are having, if not worse sleep that you are having before you started taking sleeping pills.
And the danger surround sleeping pills and their lack of true benefit above and beyond placebo, which is, if you look at these meta-analyses, in 2015 or 2016, the American College of Physicians made a landmark recommendation. They said that sleeping pills must no longer be the first-line recommended treatment for insomnia. It must be cognitive behavioral therapy for insomnia because of both the deleterious, deathly, and carcinogenic consequences of...or association with...I shouldn't say cause because we don't yet know cause. But certainly they are associated with higher mortality risk and higher cancer rates. CBTI, this cognitive behavioral therapy, must be the first-line recommendation treatment.
The problem is most doctors don't know about it because most doctors get a less than two hours of sleep education during the medical curriculum. And this is another crusade that I am on. I am desperately trying to reach out to all medical curriculum, not just here in the United States but in all nations where you have medical programs. We need a greater degree of medical education. Our doctors are not at fault at, you know, not understanding sleep. They have not been educated about sleep, you know.
So I teach a class here at University of California Berkeley. It's usually around 500 or 600 kids. It's the Science of Sleep. And they get 25, hopefully, meaningful lectures about sleep across the semester. They will have had somewhere between 10 to 15 times more sleep education than the standard doctor that you will go and see. You know, most doctors don't ask how much sleep that you're getting despite it being this fundamental, you know...Sleep is a life support system, and it is mother nature's best effort yet at immortality. And it's a key to disease, and it's a key to potentially helping treat or even prevent disease. Most doctors don't ask because most doctors aren't educated.
Rhonda: Right. Nutrition is another one of those areas.
Matt: It's right up that, you know...
Rhonda: But thankfully, we have people like you who are doing phenomenal research and also communicating that research quite nicely. I read your book. It was a really great book. It's "Why We Sleep."
Matt: Thank you.
Rhonda: So if people do want to learn more about your research, about sleep, about anything related to sleep or what you do, they can find you...
Matt: They can find me, unfortunately, all over the internet. My handle on social media is @sleepdiplomat, all one word, so @sleepdiplomat. You will find me on Twitter. You will find me sleepdiplomat.com on the web. My center here at University of California Berkeley is the Center of Human Sleep Science. If you just google that, you will find that. And there's lots of content. And if you would like an education on sleep, or you're just interested in sleep, or you're struggling with sleep, the book which has been out now and it is out now in paperback, is called "Why We Sleep." It is published by Scribner here in the United States, and it's published by Penguin back in the United Kingdom.
Rhonda: Well, Matt, thank you so much for taking some time out of your busy day to speak with me. I really really enjoyed this competition.
Matt: You're very welcome. Thank you so much for being such a wonderful sleep ambassador. You know, I am on a mission. I'm desperately trying to reach the public because I think this this message has been the neglected stepsister in the health conversation of today. But I can't do it alone. I need to partner with, you know, fantastic scientists and public figures, people like yourself who, you know, provide this platform and this forum. So I'm going to anoint you as a sleep ambassador now as well. So thank you. But just generally, thank you for this opportunity to reach your audience and speak about sleep. I really do appreciate it so much.
A catecholamine hormone produced by the adrenal glands and some neurons. Adrenaline, also known as epinephrine, exerts many effects in the body, the most notable being those associated with the “fight or flight” response to stressors. The effects of epinephrine and norepinephrine (a related catecholamine) are mediated by adrenergic receptors, which act as the interface between the sympathetic nervous system and the cardiovascular system.
Nerves that convey sensory information from the body surface, muscles, and organs to the spinal cord. Afferent nerve fibers are highly specialized, responding preferentially to a variety of stimuli. The vagus nerve (tenth cranial nerve) is composed of approximately 80 percent afferent nerve fibers that carry information from the respiratory tract, heart, and gut to the brain. In addition, the gut, microbiota, and brain communicate in a bidirectional fashion via the vagus nerve, which can sense microbiota metabolites through its afferent nerve fibers and then generate a response. One such response is an anti-inflammatory pathway that can dampen peripheral inflammation and decrease gut permeability. Stress inhibits vagal nerve activity and is involved in the pathophysiology of gut disorders such as irritable bowel syndrome and inflammatory bowel disease.
The death rate from all causes of death for a population in a given time period.
A neurodegenerative disorder characterized by progressive memory loss, spatial disorientation, cognitive dysfunction, and behavioral changes. The pathological hallmarks of Alzheimer's disease include amyloid-beta plaques, tau tangles, and reduced brain glucose uptake. Most cases of Alzheimer's disease do not run in families and are described as "sporadic." The primary risk factor for sporadic Alzheimer's disease is aging, with prevalence roughly doubling every five years after age 65. Roughly one-third of people aged 85 and older have Alzheimer's. The major genetic risk factor for Alzheimer's is a variant in the apolipoprotein E (APOE) gene called APOE4.
A prescription drug used to treat insomnia (also known as Zolpidem). Ambien is in a class of medications called sedative-hypnotics. It promotes the activity of GABA receptors in the brain, which slows brain activity to allow sleep.
An area of the brain located close to the hippocampus, in the frontal portion of the temporal lobe. The amygdala governs our responses to fear, arousal, and emotional stimulation. Poor sleep increases activity within the amygdala.
A toxic 42 amino acid peptide that aggregates and forms plaques in the brain with age. Amyloid-beta is associated with Alzheimer's disease, a progressive neurodegenerative disease that can occur in middle or old age and is the most common cause of dementia. Heat shock proteins have been shown to inhibit the early aggregation of amyloid beta 42 and reduce amyloid beta plaque toxicity [1].
Anxiety-causing substances or activities. Anxiogenic entities include drugs (such as caffeine), circumstances (such as social events or trauma), and behaviors (such as excessive engagement with social media), among others.
One of three common genetic variants of the APOE (apolipoprotein E) gene. The APOE4 allele, which is present in approximately 10-15% of people, increases the risk of developing Alzheimer's disease and lowers the age of onset. Having one copy of E4 increases risk 2- to 3-fold, while having two copies increases risk as much as 15-fold.
A division of the peripheral nervous system that influences the function of internal organs. The autonomic nervous system regulates bodily functions that occur below the level of consciousness, such as heart rate, digestion, respiratory rate, pupillary response, urination, and sexual arousal. It is the primary mechanism in control of the fight-or-flight response and the freeze-and-dissociate response.
A bidirectional cell signaling pathway that may regulate cell function, metabolism, or other aspects of physiology. Most signaling pathways are unidirectional. However, an axis may involve two or more signaling proteins and their secreting organs or cells in a type of feedback loop. For example, the growth hormone/IGF axis, also known as the Hypothalamic–pituitary–somatotropic axis, is a highly regulated pathway involving IGF-1 (produced by the liver), growth hormone (produced by the pituitary), and growth hormone-releasing hormone (produced by the hypothalamus).
An aromatic hydrocarbon compound produced during the distillation and burning of fossil fuels, such as gasoline. It is also present in the smoke from forest fires, volcanoes, and cigarettes. Benzene is a carcinogen that targets the liver, kidney, lung, heart, and brain and can cause DNA strand breaks, chromosomal damage, and genetic instability.
A highly selective semi-permeable barrier in the brain made up of endothelial cells connected by tight junctions. The blood-brain barrier separates the circulating blood from the brain's extracellular fluid in the central nervous system. Whereas water, lipid-soluble molecules, and some gases can pass through the blood-brain barrier via passive diffusion, molecules such as glucose and amino acids that are crucial to neural function enter via selective transport. The barrier prevents the entry of lipophilic substances that may be neurotoxic via an active transport mechanism.
A wavelength of light emitted from natural and electronic sources. Blue light exposure is associated with improved attention span, reaction time, and mood. However, exposure to blue light outside the normal daytime hours may suppress melatonin secretion, impairing sleep patterns. In addition, blue light contributes to digital eye strain and may increase risk of developing macular degeneration.
A cannabinoid substance present in the leaves of the marijuana (cannabis) plant. CBD is non‐psychoactive and shows potential as an anti‐inflammatory, neuroprotective, or anti-seizure drug.
A collective term for the various components of Cannabis sativa, also known as marijuana.
Clear, colorless liquid present in the brain ventricles and the cranial and spinal subarachnoid spaces. CSF provides protection for the central nervous system and plays a prominent role in brain development and neuronal functioning. CSF is renewed about four times every 24 hours. Low CSF turnover rate, which occurs with aging, leads to accumulation of catabolites in the brain and CSF – such as amyloid beta – that are often observed in certain neurodegenerative conditions such as Alzheimer's disease.
An individual’s innate tendency to sleep at a particular time during a 24-hour period. Chronotypes, which are based on circadian rhythms, are genetically determined. Disruption of a person’s chronotypic schedule can influence mood, productivity, and disease risk.
The body’s 24-hour cycles of biological, hormonal, and behavioral patterns. Circadian rhythms modulate a wide array of physiological processes, including the body’s production of hormones that regulate sleep, hunger, metabolism, and others, ultimately influencing body weight, performance, and susceptibility to disease. As much as 80 percent of gene expression in mammals is under circadian control, including genes in the brain, liver, and muscle.[1] Consequently, circadian rhythmicity may have profound implications for human healthspan.
A member of the same species.
A type of memory that occurs when contextual cues facilitate memory recall. CDM is based on the premise that during memory storage, contextual information, such as smells, tastes, or sounds, are also stored. Retrieval of the memories is enhanced when exposed to the context. Olfactory (smell) stimuli are among the strongest cues in inducing and retrieving memories.
A steroid hormone that participates in the body’s stress response. Cortisol is a glucocorticoid hormone produced in humans by the adrenal gland. It is released in response to stress and low blood glucose. Chronic elevated cortisol is associated with accelerated aging. It may damage the hippocampus and impair hippocampus-dependent learning and memory in humans.
A broad category of small proteins (~5-20 kDa) that are important in cell signaling. Cytokines are short-lived proteins that are released by cells to regulate the function of other cells. Sources of cytokines include macrophages, B lymphocytes, mast cells, endothelial cells, fibroblasts, and various stromal cells. Types of cytokines include chemokines, interferons, interleukins, lymphokines, and tumor necrosis factor.
A general term referring to cognitive decline that interferes with normal daily living. Dementia commonly occurs in older age and is characterized by progressive loss of memory, executive function, and reasoning. Approximately 70 percent of all dementia cases are due to Alzheimer’s disease.
A mood disorder characterized by profound sadness, fatigue, altered sleep and appetite, as well as feelings of guilt or low self-worth. Depression is often accompanied by perturbations in metabolic, hormonal, and immune function. A critical element in the pathophysiology of depression is inflammation. As a result, elevated biomarkers of inflammation, including the proinflammatory cytokines interleukin-6 and tumor necrosis factor-alpha, are commonly observed in depressed people. Although selective serotonin reuptake inhibitors and cognitive behavioral therapy typically form the first line of treatment for people who have depression, several non-pharmacological adjunct therapies have demonstrated effectiveness in modulating depressive symptoms, including exercise, dietary modification (especially interventions that capitalize on circadian rhythms), meditation, sauna use, and light therapy, among others.
A measure of the efficiency of a person’s glucose homeostasis. Disposition index is based on the ability of the beta cells to upregulate insulin secretion in response to a decrease in insulin sensitivity. It typically declines well before a person’s glucose levels rise into the diabetic range (126 mg/dL or greater). As such, a low disposition index is an early marker of poor beta-cell compensation and a risk factor for diabetes.
Animals characterized by higher activity during the day and sleeping more at night.
The relative ratios of the two major microbial phyla in the human gut. Firmicutes and Bacteroidetes represent 99 percent of the bacteria in the gut. However, the levels of these two dominant bacterial divisions shift in response to a variety of factors, including diet, exercise, physiological and psychological stress, and age, even when taking large inter-individual variation into account. A low Firmicutes to Bacteroidetes ratio is associated with a wide array of diseases, including metabolic dysfunction, cardiovascular disease, obesity, neurological disorders, and autoimmune disease, among others.
A neurotransmitter produced in the brain that blocks impulses between nerve cells. GABA is the major inhibitory neurotransmitter in gray matter.
The process in which information stored in DNA is converted into instructions for making proteins or other molecules. Gene expression is highly regulated. It allows a cell to respond to factors in its environment and involves two processes: transcription and translation. Gene expression can be turned on or off, or it can simply be increased or decreased.
The genetic constitution of an individual organism. The combination of genotype and environment determine an organism's physical characteristics – known as the phenotype.
A hormone produced in the gut that signals hunger. Ghrelin acts on cells in the hypothalamus to stimulate appetite, increase food intake, and promote growth. Ghrelin’s effects are opposed by leptin, the “satiety hormone.” Sleep deprivation increases ghrelin levels and feelings of hunger, which can lead to weight gain and metabolic dysfunction.
A broad class of supportive cells in the central nervous system. Glial cells surround and provide support for and insulation between neurons. Unlike neurons, glial cells do not conduct electrical impulses. Glial cells are the most abundant cell types in the central nervous system, outnumbering neurons by a ratio of roughly 3 to 1. They are generally smaller than neurons, and they lack axons and dendrites. Types of glial cells include oligodendrocytes, astrocytes, ependymal cells, Schwann cells, microglia, and satellite cells.
A system that clears the brain of metabolites and other waste. The glymphatic system comprises a vast arrangement of interstitial fluid-filled cavities surrounding the small blood vessels that serve the brain. During sleep, these perivascular structures increase in size by more than 60 percent. This allows a “flushing” operation in which waste products can be eliminated. The glymphatic system also facilitates the distribution of essential nutrients such as glucose, lipids, and amino acids, as well as other substances, such as growth factors and neuromodulators.
The years of a person’s life spent free of disease.
Relating to or characterized by pleasure. Hedonism is a school of thought that argues that pleasure and happiness are the primary or most important intrinsic goods and the aim of human life.
A small organ located within the brain's medial temporal lobe. The hippocampus is associated primarily with memory (in particular, the consolidation of short-term memories to long-term memories), learning, and spatial navigation. Amyloid-beta plaque accumulation, tau tangle formation, and subsequent atrophy in the hippocampus are early indicators of Alzheimer’s disease.
A region of the forebrain below the thalamus that coordinates both the autonomic nervous system and the activity of the pituitary, controlling body temperature, thirst, hunger, and other homeostatic systems, and involved in sleep and emotional activity.
Condition in which the body or a region of the body is deprived of adequate oxygen supply. Hypoxia may be classified as either generalized, affecting the whole body, or local, affecting a region of the body.
A critical element of the body’s immune response. Inflammation occurs when the body is exposed to harmful stimuli, such as pathogens, damaged cells, or irritants. It is a protective response that involves immune cells, cell-signaling proteins, and pro-inflammatory factors. Acute inflammation occurs after minor injuries or infections and is characterized by local redness, swelling, or fever. Chronic inflammation occurs on the cellular level in response to toxins or other stressors and is often “invisible.” It plays a key role in the development of many chronic diseases, including cancer, cardiovascular disease, and diabetes.
A peptide hormone secreted by the beta cells of the pancreatic islets cells. Insulin maintains normal blood glucose levels by facilitating the uptake of glucose into cells; regulating carbohydrate, lipid, and protein metabolism; and promoting cell division and growth. Insulin resistance, a characteristic of type 2 diabetes, is a condition in which normal insulin levels do not produce a biological response, which can lead to high blood glucose levels.
A hormone produced primarily by adipocytes (fat cells) that signals a feeling of satiety, or fullness, after a meal. Leptin acts on cells in the hypothalamus to reduce appetite and subsequent food intake. Leptin’s effects are opposed by ghrelin, the “hunger hormone.” Both acute and chronic sleep deprivation decrease leptin levels.
The long-lasting strengthening of synapses (connections) between nerve cells. LTP is associated with the learning and memory functions of the hippocampus and other structures in the brain. It allows nerve cells that fire in a correlated manner in a given activity to increase their connection strength with each other, while decreasing the strength of connectivity between neurons that do not take part in the activity.
An enzyme that participates in genetic pathways that sense amino acid concentrations and regulate cell growth, cell proliferation, cell motility, cell survival, protein synthesis, autophagy, and transcription. mTOR integrates other pathways including insulin, growth factors (such as IGF-1), and amino acids. It plays key roles in mammalian metabolism and physiology, with important roles in the function of tissues including liver, muscle, white and brown adipose tissue, and the brain. It is dysregulated in many human diseases, such as diabetes, obesity, depression, and certain cancers. mTOR has two subunits, mTORC1 and mTORC2. Also referred to as “mammalian” target of rapamycin.
Rapamycin, the drug for which this pathway is named (and the anti-aging properties of which are the subject of many studies), was discovered in the 1970s and is used as an immunosuppressant in organ donor recipients.
A hormone that regulates the sleep-wake cycle in mammals. Melatonin is produced in the pineal gland of the brain and is involved in the expression of more than 500 genes. The greatest influence on melatonin secretion is light: Generally, melatonin levels are low during the day and high during the night. Interestingly, melatonin levels are elevated in blind people, potentially contributing to their decreased cancer risk.[1]
The collection of genomes of the microorganisms in a given niche. The human microbiome plays key roles in development, immunity, and nutrition. Microbiome dysfunction is associated with the pathology of several conditions, including obesity, depression, and autoimmune disorders such as type 1 diabetes, rheumatoid arthritis, muscular dystrophy, multiple sclerosis, and fibromyalgia.
A phase of sleep characterized by slow brain waves, heart rate, and respiration. NREM sleep occurs in four distinct stages of increasing depth leading to REM sleep. It comprises approximately 75 to 80 percent of a person’s total sleep time.
One of the two main divisions of the autonomic nervous system (the other being the sympathetic nervous system). The parasympathetic nervous system's primary function is to control homeostasis and the body at rest. It conserves energy as it slows the heart rate, increases gut motility and hormonal activity, and relaxes sphincter muscles in the gastrointestinal tract.
The observable physical characteristics of an organism. Phenotype traits include height, weight, metabolic profile, and disease state. An individual’s phenotype is determined by both genetic and environmental factors.
The area of the brain located in the front portion of the frontal lobe, just behind the area commonly known as the forehead. The prefrontal cortex is involved in a variety of higher cognitive functions and behaviors such as executive function and expression of appropriate social behavior.
A distinct phase of sleep characterized by eye movements similar to those of wakefulness. REM sleep occurs 70 to 90 minutes after a person first falls asleep. It comprises approximately 20 to 25 percent of a person’s total sleep time and may occur several times throughout a night’s sleep. REM is thought to be involved in the process of storing memories, learning, and balancing mood. Dreams occur during REM sleep.
Good health. A person in rude health is full of vigor and free of illness.
A small molecule that functions as both a neurotransmitter and a hormone. Serotonin is produced in the brain and gut and facilitates the bidirectional communication between the two. It regulates many physiological functions, including sleep, appetite, mood, thermoregulation, and others. Many antidepressants are selective serotonin reuptake inhibitors (SSRIs), which work by preventing the reabsorption of serotonin, thereby increasing extracellular levels of the hormone.
A person who works on a schedule outside the traditional 9 AM – 5 PM day. Work can involve evening or night shifts, early morning shifts, and rotating shifts. Many industries rely heavily on shift work, and millions of people work in jobs that require shift schedules.
A sleep disorder characterized by repeated interruptions in breathing during sleep, reducing oxygen levels and disrupting sleep patterns. Two primary types of apnea have been identified: obstructive sleep apnea (OSA, caused by airway blockage) and central sleep apnea (CSA, caused by the brain's failure to signal breathing). Sleep apnea causes brain hypoxia and has been associated with an increased risk of many serious health conditions, including hypertension, cardiovascular disease, diabetes, depression, and stroke.[1]
Sudden bursts of brain electrical activity that resemble spindles when recorded on an electroencephalogram. Sleep spindles occur during non-rapid eye movement (NREM) sleep and are believed to mediate many sleep-related functions, from memory consolidation to cortical development.
A diagnostic tool used in sleep medicine. During a sleep study, a person’s brain activity, eye movements, muscle activity, and heart rhythm are recorded. Sleep studies can determine quality of sleep and identify sleep disorders, such as apnea.
Sleep-promoting substances or activities. Somnogenic entities include exercise, meditation, and illness, among others.
A substance or activity that induces sleep. Soporifics include drugs, endogenous substances, meditation, and the lowering of lights in a room.
A type of polysaccharide – a large carbohydrate consisting of many glucose units joined by glycosidic bonds. Starch is produced by plants and is present in many staple foods, such as potatoes, wheat, maize (corn), rice, and cassava. It is the most common carbohydrate in human diets. Pure starch is a white, tasteless, and odorless powder.
One of the two main divisions of the autonomic nervous system (the other being the parasympathetic nervous system). The sympathetic nervous system's primary process is to stimulate the body's fight-or-flight response. It is constantly active, however, at a basic level to maintain homeostasis. The sympathetic nervous system is described as being complementary to the parasympathetic nervous system which stimulates the body to "rest-and-digest" or "feed-and-breed".
A microtubule-bound protein that forms the neurofibrillary "tau tangles" associated with Alzheimer's disease. Tau tangles disrupt transport of metabolites, lipids, and mitochondria across a neuron to the synapse where neurotransmission occurs. Diminished slow-wave sleep is associated with higher levels of tau in the brain. Elevated tau is a sign of Alzheimer's disease and has been linked to cognitive decline.
Abnormal aggregates of hyperphosphorylated tau, a protein found in the brain. Tau tangles are associated with traumatic brain injury and chronic traumatic encephalopathy and are one of the defining characteristics of Alzheimer’s disease. They inhibit normal brain function, and the degree of cognitive impairment in diseases such as Alzheimer’s is significantly correlated with their presence.
Distinctive structures comprised of short, repetitive sequences of DNA located on the ends of chromosomes. Telomeres form a protective “cap” – a sort of disposable buffer that gradually shortens with age – that prevents chromosomes from losing genes or sticking to other chromosomes during cell division. When the telomeres on a cell’s chromosomes get too short, the chromosome reaches a “critical length,” and the cell stops dividing (senescence) or dies (apoptosis). Telomeres are replenished by the enzyme telomerase, a reverse transcriptase.
The primary male sex hormone. Testosterone is critical to the maintenance of fertility and secondary sexual characteristics in males. Low testosterone levels may increase risk of developing Alzheimer’s disease.
The primary psychoactive substance present in the leaves of the marijuana (cannabis) plant. THC alters the functioning of the hippocampus and orbitofrontal cortex, leading to altered perception and changes in cognition, such as short-term memory impairment. THC’s chemical structure is similar to the brain’s endogenous cannabinoid anandamide, allowing it to bind to anandamide receptors to elicit its effects.
An essential amino acid. Tryptophan plays key roles in the biosynthesis of proteins and is a precursor to several molecules with physiological significance, including melatonin, niacin, and the neurotransmitter serotonin. Inflammation causes tryptophan to be reallocated from serotonin synthesis to that of kynurenine, which then converts to the neurotoxin quinolinic acid, leading to depression. Dietary sources of tryptophan include most protein-based foods, such as meat, beans, or nuts.
Coinciding with reality. Veridical memories decrease with age, especially in the setting of dementia. "False memories" are non-veridical.
Member only extras:
Learn more about the advantages of a premium membership by clicking below.
Supporting our work
If you enjoy the fruits of
 , you can participate in helping us to keep improving it. Creating a premium subscription does just that! Plus, we throw in occasional member perks and, more importantly, churn out the best possible content without concerning ourselves with the wishes of any dark overlords.
, you can participate in helping us to keep improving it. Creating a premium subscription does just that! Plus, we throw in occasional member perks and, more importantly, churn out the best possible content without concerning ourselves with the wishes of any dark overlords.
Sleep News
- High-intensity exercise in the evening may be associated with greater reductions of the hunger stimulating hormones
- The lullaby of the sun: the role of vitamin D in sleep disturbance. - PubMed - NCBI
- Microbiome Analysis Powers Insights to Improve Sleep
- Older people who have less slow-wave deep sleep were shown to have higher levels of tau tangles in the brain which is linked to Alzheimer's disease.
- Caffeine that was given to people 3 hours before normal bedtime caused a 40-minute shift in the body's internal clock.




















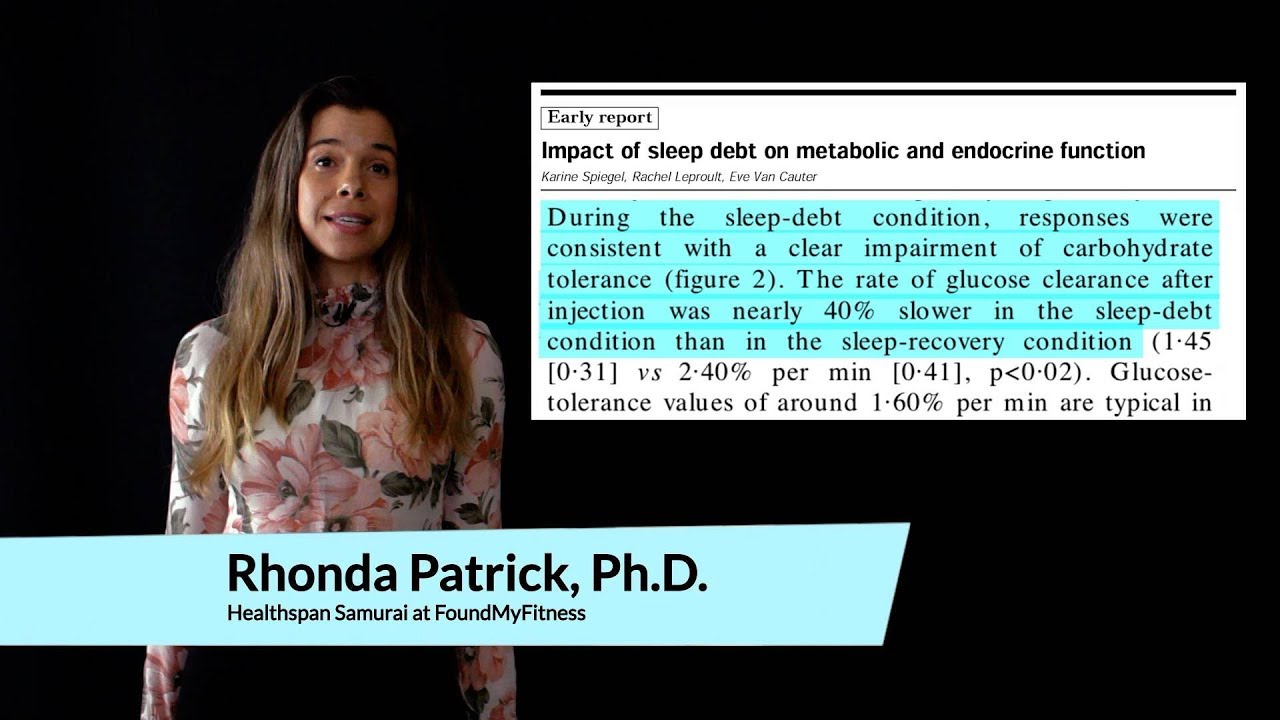









I’m reachable for each incalls in my lavishness flat or outcalls all through metropolis City Gurgaon And Delhi. My personality is nice natured, therefore I am constantly patient and thoughtful.i’m dedicated to making sure that you simply become a glad shopper which you may need me again and again. http://www.escortsnights.com/
I’m confused about one of the early descriptions of an increase in sleep spindles supposedly consolidating the motor development occuring from around 12 months. Scholle et al. (2007) state “Between age 1.1 and 3 years the spindle density was lowest and the interspindle interval was longest with high variability; at this time also, the spindle length was shortest”. Low spindle density, long interspindle intervals and short spindle length sounds to me like a decrease in sleep spindles???
Thank you so much for a fantastic interview! Sorry I’m late to the discussion on this episode. Hopefully someone will still see this…
I’ve been following a few of Dr. Walker’s interviews lately, and I’m becoming more and more concerned for my future mental health.
I was diagnosed with narcolepsy at age 15. I’m about to be 32. I have most of the classic symptoms of the disease including excessive daytime sleepiness, cataplexy, sleep paralysis, vivid dreaming, and irregular NREM/REM patterns. The most alarming as it relates to Dr. Walker’s research is the lack of deep NREM sleep. In two clinical sleep studies (the first at initial diagnosis at age 15, and again about 1.5 years ago) I almost entirely skipped past stages 3 and 4 NREM. In a couple sessions I went from full consciousness to REM sleep in under 1 minute.
At two different stages of my life I have tried Xyrem to supplement my deep sleep at night. Long story short: I had a bad sleep paralysis episode that made me not want to continue use.
So, if you’ve made it this far, what can I do to help improve the amount of NREM sleep I get (aside from drug induced sleep)? I have a pretty well regulated sleep/wake schedule, I do CrossFit 3 times a week, eat clean (and try to prevent late meals), I have a very bright office, and I don’t use electronics much at all during the evening. Any help is welcome.
Thanks again for a great interview!
I sleep on a Japanese mattress. My girlfriend hates it. I like a firm surface. I want to know what is the best bedding material for a good night sleep. I often sleep on the floor when I am a guest in peoples house. I feel like I fall asleep faster and stay asleep more. I am concerned that I am just psycho somatizing perceived benefits from my boutique-y hand made Japanese mattress. I saw this designer bed that was based on the chimpanzee’s nest design that touted a paleolithic sleep experience as it’s selling point.
I have slow choline metabolism gene polymorphism, one copy of aloep4, and the other one that limits deep sleep. I think it’s really hard for me to not use digital entertainment near bedtime is my sleep problem. I wear blue blockers, I have a pitch black room, and I turn off all the electronics when i do go to sleep. I often wake up early like around 6, I ussually have energy and feel pretty well rested. It is rare for me to exceed 7 hrs of sleep. I noticed using mouth tape for my nose breathing has increased my restfulness. The earliest I can manage to go to bed avoiding lights is around 1015, typically I will get there around 11. I take magnesium, zinc, collagen, i avoid sugar, i avoid seed oils, i limit carbs. I think i need to sauna more and drink less coffee. coffee is the one thing I do. it’s my only vice. i have so many food abstentions. I have a problem with under eating as well, I rarely have much appetite. There are so many variables to consider. I have had sleep difficulty for the past 10 years or so and it’s gotten better this past year trying these strategies. it is a challenge trying to put all of it into practice, especially meditation.
The best sleep i get is when i am back packing for more than 2 weeks. I sleep 8 pm to 7 am after hiking all day in constant sunlight exposure.
Does the found my fitness dna assessment detail chronotype gene polymorphisms?
What a stellar interview!
One question I was left with is regarding chronotypes. Dr. Walker mentioned that many people think they are of one chronotype, but genetically they are not.
How does someone determine which chronotype they are? Is this identifiable in standard genetic testing?
Hi Lars86,
There are certain genes that code for chronotype, also named ‘clock genes’ as they activate processes in our biological clock. These are mainly the genes PER1, PER2 and PER3 (which are most often investigated in scientific research). Chronotype itself, however, is examined with a questionnaire in most scientific studies. A famous (and validated!) questionnaire used for is the Munich Chronotype Questionnaire (MCTQ). You can find the questionnaire and calculation of the score here: https://www.thewep.org/documentations/mctq The score is based on self-reported average bedtimes, sleep times, and wake times on working days and free days.
That said, I do not fully agree with what Matthew Walker is saying about “you cannot do something about your chronotype, it is genetic”. I totally believe that there is a genetic component in your chronotype, but based on what I have read (I am a postdoc researcher studying the effects of light on alertness, performance, and sleep myself) I think the environment is basically creating ‘late chronotypes’ nowadays. Take a look at this study for example: https://www.sciencedirect.com/science/article/pii/S0960982213007641 They investigated chronotypes (circadian phase) in people who were ‘forced’ to go camping under natural light only for one week (no artificial light sources were allowed or present). The timing of the internal clocks of the late chronotypes in this study became more similar to the internal clocks of the early chronotypes, just after one week of camping under natural light exposure. I think the variation in chronotypes would be much smaller if we would have continued living under natural light exposure only. Light pollution at night and too low levels of light during the day are creating late chronotypes.
Fascinating information. What is Dr. Walker’s advice regarding melatonin supplements? Can melatonin supplements increase the deep sleep duration in older people?
Awesome interview and information. Thank you, Rhonda!
Related: L-Serine http://fortune.com/longform/alzheimers-disease-cure-breakthrough/