#64 Dr. Michael Snyder on Continuous Glucose Monitoring and Deep Profiling for Personalized Medicine
This episode is available in a convenient podcast format.
These episodes make great companion listening for a long drive.
The BDNF Protocol Guide
An essential checklist for cognitive longevity — filled with specific exercise, heat stress, and omega-3 protocols for boosting BDNF. Enter your email, and we'll deliver it straight to your inbox.
Dr. Michael Snyder, the chairman of the Department of Genetics and director of the Center for Genomics and Personalized Medicine at Stanford University, is a pioneer and powerful advocate in the field of "wearables," electronic devices that patients or consumers can wear to monitor their health, fitness, activity, sleep, or even mood. Wearable devices can transmit information to a physician or user in real time, allowing the wearer to actively participate in monitoring and maintaining their own health. The proud bearer of eight wearables, Dr. Snyder describes himself as one of the most extensively monitored scientific researchers, a firm believer that "more is better" when it comes to data.

With increasingly precise tracking, the future of medicine may be one in which early insights gathered from emerging clinical tools and common consumer wearables fundamentally change a person's health trajectory – a stark contrast from the confining, too-little-too-late, reactive approach of traditional medicine.
Data on the genome, transcriptome, proteome, metabolome, and more lend insights on disease vulnerabilities that might lead to more effective and/or timely treatment and intervention. In his case, he identified a personal susceptibility that didn't fit with what he expected from his phenotype – a surprising diagnosis of type 2 diabetes.
In this episode, Dr. Snyder and I discuss:
-
How Dr. Snyder's genomic analysis revealed he was at risk for type 2 diabetes.
-
How some of Dr. Snyder's data suggest that nine out of ten people with pre-diabetes are unaware they have it.
-
How a person's blood glucose response to a specific type of food can differ markedly from another person's.
-
How Dr. Snyder used wearable devices to help diagnose his Lyme disease.
-
How Dr. Synder's ongoing study uses wearable devices to help identify elevated heart rate as one of the first symptoms in many illnesses, including COVID-19.
-
How smartwatches that can detect heart rate variability may help detect some heart conditions such as atrial fibrillation – a forerunner for heart disease.
-
How measuring a person's exposome can identify what airborne pathogens they've been exposed to and what this means for disease risk.
-
How children exposed to high levels of air pollution have biomarkers of Alzheimer's disease in their brains.
-
How certain lifestyle modifications such as sauna use and sulforaphane intake can help rid the body of some airborne pollutants.
-
How Dr. Snyder's data suggest that organs such as the heart, liver, and kidneys age at different rates in different people and how this may define how people age and what diseases they are more susceptible to.
-
How the gut microbiome influences glucose regulation and cholesterol.
Continuous glucose monitors for personalized medicine
"It's pretty clear that nine out of ten people who have pre-diabetes…actually have no idea." - Dr. Michael Snyder Click To Tweet
Type 2 diabetes is a complex constellation of interrelated metabolic conditions characterized by high blood glucose levels. A precursor to the disease is prediabetes – a condition in which blood glucose levels are higher than normal, but not high enough to indicate a diagnosis of type 2 diabetes. Experts estimate that more than 88 million people living in the United States (roughly one-third of the population) have prediabetes. The condition can be halted or reversed with dietary and lifestyle modifications, including weight loss, exercise, and stress reduction. But most people with prediabetes don't know they have the disorder until it has transitioned to diabetes.
Wearable devices that have garnered a lot of attention in recent years are continuous glucose monitors, or CGMs for short. These small electronic devices allow users to monitor their blood glucose levels in more or less real-time, through a tiny sensor placed on the skin where it samples from the interstitium rather than the blood.
Although CGMs were originally designed for people who have diabetes, the devices have taken on tremendous value as diagnostic tools – helping to not only identify the vast numbers of people who have prediabetes or diabetes, but also provide those not clinically affected by diabetes with a way to receive near-instant feedback on their dietary glucose response. CGMs can also yield unexpected insights as scientists like Dr. Snyder divine a way to use the broader patterns of glucose regulation as a means to identify non-dietary factors, such as viral infection or stress, that can markedly increase blood glucose levels. Since maintaining consistent, moderate blood glucose levels is the key to maintaining long-term metabolic health, CGMs may be a powerful weapon in thwarting what has become a growing public health problem.
Mending a broken healthcare system with preventive medicine
But identifying people who have prediabetes is just one example of how wearable devices and extensive biomonitoring can be used to paint a more accurate, comprehensive picture of a person's health. Rather than relying on blood tests performed just once a year (or less often) during a routine physical, measurements derived from biospecimens and wearable devices have the advantage of providing up-to-the-minute assessments of the thousands of physiological processes occurring in the human body and identifying when things go wrong – in the moment. Such knowledge offers the promise of early diagnosis or even prevention of cancers, cardiovascular diseases, and metabolic dysfunction in their earliest stages.
Biomonitoring through common wearables to detect early infection
Dr. Snyder's experiences with analyzing his own data, as we discuss in this episode, and identifying signals that indicated he had been ill prompted him to develop an algorithm that used changes in a person's heart rate as a bellwether of acute illness. He and his colleagues are now investigating the algorithm's use in identifying whether a person might have COVID-19. The early data are promising, having demonstrated that more than 80 percent of people who have COVID-19 have an increase in heart rate early in the disease process. Such a finding could have tremendous public health benefits, alerting people to the fact that they are ill so they can self-quarantine.
A totality of non-genetic tangible exposures
[tweetbox text='"…the ultimate goal is to try and understand how exposures will contribute to your disease [risk]. Because there's no question that your risk for disease depends upon genetics, but it also depends upon [your] environment." - Dr. Michael Snyder Click To Tweet
Another wearable, an investigative research tool developed by Dr. Snyder's group, attempts to measure a person's airborne and chemical exposome, the totality of non-genetic tangible exposures a person experiences during a lifetime, including those from air, physical surroundings, microbes, and chemicals. Because many of the things a person breathes and is exposed to are carcinogenic or carry other risks, the exposome can have myriad effects on one's health. Assessing one's genetic and environmental exposures can paint a clear picture of disease risk and help drive informed decisions about diet and lifestyle to mitigate some of that risk.
As the human body ages, massive shifts in the proteome occur, correlating with distinct biological pathways and revealing associations with age-related diseases and phenotypes. Understanding these and other molecular changes has the potential to reveal unique signatures and pathways that might offer targets for preventing age-related diseases.
In this episode, Dr. Michael Snyder describes his personal journey with biomonitoring and wearable devices and discusses the future of personalized medicine through the use of technology.
Sign-up for Stanford Innovation lab's COVID-19 wearable detection study

This episode was fiscally sponsored through The Film Collaborative and a grant from a generous anonymous donor.
It may be possible to detect infection pre-symptomatically using extremely common health data gathered by smart devices you may already have. If you have any of a number of common consumer fitness or health trackers, you may be eligible to join Dr. Snyder and colleagues COVID-19 detection study. Some of the wearables they support in combination with certain smartphones, include:
- Fitbit
- Garmin
- Apple Watch
- Oura
- Motiv
COVID-19 Wearables Study
Relevant publications
- A longitudinal big data approach for precision health
- Integrative omics for health and disease
- Digital Health: Tracking Physiomes and Activity Using Wearable Biosensors Reveals Useful Health-Related Information
- Glucotypes reveal new patterns of glucose dysregulation
- Personal aging markers and ageotypes revealed by deep longitudinal profiling
- Molecular Choreography of Acute Exercise
Learn more about Dr. Michael Snyder
-
How Dr. Michael Snyder's genomic analysis revealed he was at risk for type 2 diabetes.
-
How some of Dr. Snyder's data suggests 9 out of 10 people with pre-diabetes are unaware they have it.
-
A person's blood glucose response to a specific type of food can differ markedly from another person's.
-
How you can use deep profiling and "big data" including genomic data, RNA data, proteomic, metabolomic, lipidomic, and microbiome data to get a better understanding of a person's health status. 1
-
How Dr. Michael Snyder used wearable devices to help diagnose his Lyme disease.
-
How Dr. Snyder's ongoing study used wearable devices to help identify elevated heart rate as one of the first symptoms in many illnesses, including COVID-19.
-
Dr. Snyder's study for early detection of diseases such as COVID-19 using smart-watch data.
-
How smart watches that can detect heart rate variability may be able to help detect some heart conditions such as atrial fibrillation.
-
How measuring a person's exposome can identify what airborne pathogens they've been exposed to and how Dr. Snyder is trying to determine what this means for disease risk.
-
How children exposed to high levels of air pollution have biomarkers of Alzheimer's disease in their brains. 1
-
How certain lifestyle modifications such as sauna use and sulforaphane can help rid the body of some airborne pollutants.
-
How sulforaphane can increase benzene excretion by up to 60%. 1
-
How some heavy metals such as cadmium and mercury are robustly excreted through sweat. 1
-
Dr. Snyder's data suggests that organs such as the heart, liver, kidneys, etc. age at different rates in different people and how this may define how people age and what diseases they are more susceptible to. 1
-
The scientific interest in researching metformin as a potential longevity drug. 1
-
How metformin blunts exercise-induced benefits in healthy older adults without type 2 diabetes. 1
-
Dr. Snyder's data showed that exercise induces thousands of molecular changes in genes that regulate energy metabolism, oxidative stress, inflammation, immune function, tissue repair and more. 1
-
How aging is driven by both genetic and lifestyle factors.
-
How the gut microbiome influences glucose regulation and cholesterol.
Dr. Patrick: Welcome back to another episode, everyone. I'm super excited to be sitting here with Dr. Michael Snyder who is the chair of the Department of Genetics, and the director of the Center for Genomics and Personalized Medicine at Stanford. He also runs a team of over 100 scientists at the Innovation Lab at Stanford, which we're going to talk probably in great detail about a lot of the really exciting research going on there. He and his collaborators are doing just some amazing research that will change the healthcare system, from one that's focused on treatment to one that's focused on prevention, in addition to treatment.
He's also the founder of a variety of companies. One, Q Bio, which gathers tons and tons of data, which we'll talk a little bit about this "big data." And it helps...you know, getting all these pieces of data helps give people a better understanding of their health status. He also is the founder of January AI, which is a glucose monitoring company, which we'll also get into details about.
So I, kind of, wanted to kick off this podcast, Mike with a quote from William Thompson, who is a famous...he was a famous mathematician and physicist. He basically formulated the first and second laws of thermodynamics. And he's got this quote that I've often referred to because I just think it's a great quote. And the quote is, "If you can't measure it, you can't improve it." And I feel, like, that's so relevant to your work and particularly, even to yourself. I mean, you are probably one of the most extensively monitored humans there are in modern-day. I mean, you've measured everything. I mean, people can't even imagine all the things you've measured on yourself. Maybe you could talk a little bit about what sort of parameters you've measured in yourself and what you've learned from that data.
Dr. Snyder: Yeah, sure. So we're all about collecting data. I'm a believer you can't have enough data. More information is always better than less information. So what do we collect? Well, we do deep molecular measurements on me. Well, for example, we sequence, first of all, my DNA so I know what kinds of risk factors I might have, genetic risk factors. We also do very deep molecular measurements on me. Meaning we'll draw my blood and urine profile -- literally tens of thousands of molecules. We'll study my poop for the microbiome. And we do a lot with wearables that we'll, I'm sure, talk about today with smartwatches and other devices. In fact, I have eight of those devices I use every day.
Dr. Patrick: You've actually got a pretty interesting story. So you've sequenced your entire genome and you've learned some really interesting predispositions that you have and that actually turned out to be a pretty interesting story. Do you mind talking about that a little bit?
Dr. Snyder: Sure, yeah, no, actually, this big data collection has helped me several times. And the first was, in fact, from my genome sequence. So I sequenced my genome, it told me things I was at risk for. One of them was quite surprising, it said type 2 diabetes. And I'm not overweight, I exercise pretty regularly. And I thought well, you know, how can that be? I don't have a family history of type 2 diabetes so I wasn't too sure it was right. But I was, in fact, tracking my sugar levels, which is what happens when you get type 2 diabetes, your sugar levels go up as well as many other things.
And what we discovered actually, about nine months into the study after I sequenced my DNA we saw this risk from type 2 diabetes, my sugar actually was shooting up through the roof. And I was only following closely because of the fact that my genome told me I was at high risk. And in fact, when I first discovered this, I was going in getting a test for something called insulin resistance which is associated with type 2 diabetes. And the doctor actually, you know, she was skeptical, "Why are you here? You don't look, like, you have diabetes because I'm not overweight, you don't have family history, you know, doesn't make any sense." And I said, "Well, my genome said I have this going on."
And so she actually drew blood and my sugar levels were high actually, we were both surprised. In fact, she repeated the measurements and sure enough, they were quite high. And then it turns out there's insulin resistance. I wasn't insulin resistant. I was insulin sensitive. But my sugar was high so we measured it a week later and did some other tests, something called hemoglobin A1C. And sure enough, I had crossed the threshold and was classified as type 2 diabetic. So my genome tipped me off and then these other measurements actually, you know, basically discovered it.
What was pretty unusual about it was that it came up after a very nasty viral infection actually. About three weeks later, is when I was getting measured and that's when my sugar levels were rising. It's very relevant to the current pandemic, in fact, because a lot of people think that COVID might trigger type 2 diabetes. In fact, there's some evidence for that already. But this is the first demonstration that a viral infection could actually trigger a type 2 diabetes. And so in my case, I caught it because I was doing this deep profiling.
Dr. Patrick: So how common is it that you find people that are like yourself, I mean, I typically...you know, when you see someone who's healthy, active, you know, looks lean, how common is it to see that they may be metabolically unhealthy in terms of at least, you know, their glucose regulation?
Dr. Snyder: Yeah, well, on the glucose side, it's quite frequent actually. So we have some studies going on with something called continuous glucose monitoring. But backing up a little bit, it's pretty clear that actually, 9 out of 10 people who have pre-diabetes, so not yet diabetes, actually have no idea. What that means is their glucose is starting to go out of control. They're not officially classified as diabetic yet, but they will be. And it turns out that 9% of the U.S. population is diabetic, but 33% are pre-diabetic. And most of those pre-diabetic will go on to become diabetic and yet, they have no idea they're pre-diabetic. And so we think actually capturing that information is pretty darn important so that they can start getting their glucose under control long in advance of getting full-blown type 2 diabetes.
Dr. Patrick: Now, this is something that I would imagine a routine, you know, checkup that people do, I mean, maybe they don't do this once a year or twice a year where you're getting something like, I guess. Would that even be reflected on HbA1c, which is your, sort of, long-term glucose measurements? And also you know, if there are so many people that have what are pre-diabetes...and maybe you can sort of...I don't know if you can tell us what those levels are, and if it's a pretty hard...I mean, is there a scale that's, kind of, sliding, or is it like, this is, like, for sure if you're within this range you're pre-diabetic? And also I, kind of, want to get into you know, what you've been doing with your work at Innovation Lab in terms of, like, measuring using continuous glucose monitors, which you know, a lot of people are now using these days to actually inform people about their glucose regulation.
Dr. Patrick: Continuous glucose monitors are still considered a medical device... for that reason, they are prescribed under the care of a physician. However, increasingly, they're fairly commoditized with companies like NutriSense, January.AI and Levels, making them available to virtually anyone through a physician network and selling them usually for around a couple hundred dollars per month with the most well-known CGM brands being the Dexcoms and the Freestyle Libre.
Dr. Snyder: Well, as far as range, yeah, there is. So normally people want to have their glucose at 90 or below. And when it gets over 120, then you're typically classified as type 2 diabetic. And so in between is typically called pre-diabetes. They are arbitrary numbers because it's a scale people...you know, you can be anywhere in that range. So the goal is to keep your glucose numbers down. But it's actually even more complicated than that because people will spike to foods and different foods can spike you very much out of control. So for example, if I eat pulled pork, believe it or not, that'll send my glucose over 350, it goes totally out of control.
So you do want to know what foods do that to you. It turns out that it's different for different people. So different foods by different people. And these continuous glucose monitors, which is one of the things we are using in our study is a great way to measure those. So we can actually dive deeper on that if you want. Turns out everybody spikes to different foods differently. Some people spike to bread, other people to bananas, other people to pasta, and it's just different with different people. It's thought that at least part of that's due to what's called your microbiome, the microbes in your gut that digest your food differently. And so we're all different.
And so that's why it's really important to get these personal measurements and that's a big theme of ours. Try to collect big data because everybody's different and those data will be different for different people. And so understanding people's baseline and then how they're shifting from that baseline is absolutely critical for understanding your health.
Dr. Patrick: What do you think about people that are...I mean, obviously, using continuous glucose monitors for people that are diabetic, type 1 or type 2, or for pre-diabetic. What do you think about for just the general population? I mean, there's a lot of companies now popping up that are doing, you know, just that -- allowing, you know, just normal people, like I, myself, where you and I have discussed previously in another conversation, and I've gathered a lot of data but I, sort of, want to know what your thoughts are on...?
Dr. Snyder: Well, I think everybody should wear one. Now, I'm biased, I'm a guy who likes to collect a lot of data around these things. But what's really clear, it comes back to what I was saying before, for pre-diabetics, they have no idea most of the time. They have no idea they're spiking away. And so putting these monitors on, first of all, they discover that, but even normal people, it turns out, will be spiking as well. And it has to do with the way we currently measure glucose dysregulation. We look at final glucose levels, like, we started talking about, or this hemoglobin A1C, these final levels. But there's actually different ways to have different glucose dysregulation. My own belief is diabetes is probably 50 different diseases when you lump it all together into one or two, basically, whether you have type 1 or type 2. And the reality is there's many subtypes. I'm a very unusual type 2 diabetic, actually. So these monitors are great for discovering people who have glucose dysregulation, but it doesn't show up by normal means.
They're also phenomenal because as I say people spiked to different foods. So you get to see what foods you will spike to and then you can actually personalize your habits. If you spike to bread, for example, well, maybe you want to avoid bread and eat other things. And so one of the companies I was involved in founding that's exactly what they do. They have a food recommender that says if you, you know...this is what you normally spike to, don't eat that when you go to the restaurant, eat something else that won't cause this. And I think getting taught those habits early before you're diabetic is absolutely huge. Because I think the key is to get things under control before you have disease. And that's a big theme of ours, try to catch disease early before symptoms so you can manage it and keep people healthy, basically.
Dr. Patrick: So you mentioned something very interesting that you think diabetes is, like, 50 different diseases. Can you just elaborate a little bit about that? That's very interesting.
Dr. Snyder: Yeah, so most people think, oh, you're diabetic because your cells don't respond to insulin. This is what's called insulin resistance and that's true for a lot of people. But I'm an exception, and I'm not alone, I know there are others. My cells actually respond fine to insulin. Other people are diabetic because they don't make insulin. The classic case is type 1, but there are cases of type 2 where they don't make insulin. Turns out, I make insulin fine. So I'm making insulin, my cells respond to it, so what's wrong with me? Well, it turns out I don't release it from my pancreas, which we only found by doing some pretty simple tests, actually.
And so what's needed to treat me is very different from what's needed to treat others. Turns out I'm not a metformin responder. So I don't respond to the most common type 2 diabetes drug that's out there. But I respond really great to this other drug it's called repaglinide that actually promotes release of insulin from your pancreas. So this is a classic case of knowing exactly what's wrong with you can actually suggest the right therapy, and therefore I can take medicines that will work on me, not ones that don't work on me.
So we think that's the power of all of this -- knowing exactly what's wrong. So I don't know what type of diabetic I am. I'm probably type X. Right now, I'm lumped in as type 2 but that's only because they put people in these broad categories. And I imagine there's other types as well if you look at...some people have high other kinds...like high lipids and other people don't. And that's clearly associated with more total metabolic dysregulation. And so what's probably going on with them is a little bit different from others who may not have lipid dysregulation. So it's going to vary from person to person. And so I think understanding exactly what's wrong with people will help let them manage their health much better.
Dr. Patrick: Absolutely. So you wear a continuous glucose monitor, have you found certain dietary and/or lifestyle decisions make a big impact on your glucose regulation?
Dr. Snyder: Yeah, totally. So certain foods I avoid, like the pulled pork I mentioned earlier.
Dr. Patrick: Is that...I'm sorry, the pulled pork...because, like, I eat...you know, protein and fat for me doesn't raise my postprandial glucose levels much at all. Is it just pulled pork or is it, like, sugary barbecue sauce on the pulled pork?
Dr. Snyder: Yeah, turns out there was sugar in the pulled pork. You hit the nail on the head. Everybody said to me...when I showed this as someone said, "Well, Mike, of course, everybody knows they put sugar in the pulled pork." But I had no idea. And I think we all have those eye-opening moments when you wear a continuous glucose monitor. In hindsight, it always makes sense. You're still surprised when you see it because you didn't realize that it was going on because nobody has every food memorized.
And we saw one case of...I was talking to a journalist who said he was trying to eat really healthy. He had salmon on a salad every day. And he said, you know, he couldn't think of anything healthier than that. And then his sugar spiked through the roof. And it turns out it was he had some balsamic salt on it that had sugar in it. And the same thing in hindsight he said, "Oh, of course." But he didn't realize that at the time. We all have these habits that probably has some not-so-healthy things snuck in there even when we think we're being perfectly healthy to avoid.
So anyway food avoidance, you know, or eating better foods for you is one easy thing to do. Another thing to do is exercise. I know it sounds obvious, but it's very obvious when you're wearing a glucose monitor. In fact, I can teach people as part of this app, January AI, where you actually eat something...nearly everybody spikes to rice, by the way. White rice is kind of nasty, it spikes people.
Dr. Patrick: Oh totally, I avoid it like the plague.
Dr. Snyder: So does corn flakes and milk, yeah, also pretty nasty, actually. Yeah, so that's good. Anyway, so as one training exercise, you'll eat white rice and then go eat white rice and then do a brisk walk 15 minutes later, you'd be amazed at how much it suppresses your glucose spikes. So you can actually learn these habits just either on your own by wearing a monitor or some of these apps that are out there now and programs are meant to help teach you, help you modify your behavior. So again, you can be healthier. And then the goal is to get in healthy habits so that you will be living a healthy life basically.
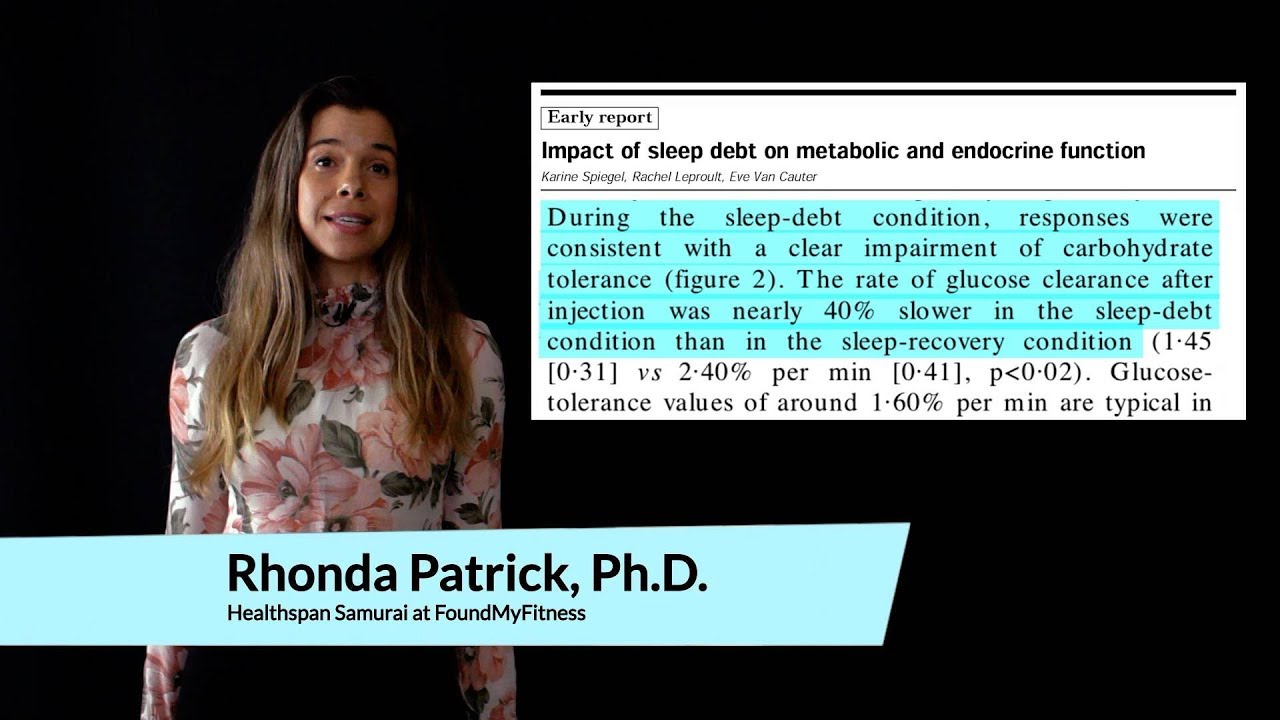
Dr. Patrick: Great. So we, kind of, took a deeper dive into the continuous glucose monitors, which I'm also a huge fan of. I've been measuring mine for the past, you know, three or something years, about three years, and learned a lot from it as well in terms of foods that, you know, have a bigger spike to, postprandial spike to. And other lifestyle factors that affect my fasting blood glucose, particularly sleep and lack of sleep, that was a big one was very, like, eye-opening for me.
But you know, through your research and your collaborators you guys are collecting not only glucose, using continuous glucose monitors to get, you know, information about people's glucose regulation. But you guys are getting a ton of data. I mean, just everything from antibodies to RNA to their proteome to metabolome. Do you mind, kind of, talking a little bit about this big data and how you're sort of longitudinally, you know, gathering all this data from people and learning interesting things about the health status of people that you hadn't...that people didn't even know about before?
Dr. Snyder: Yeah, sure. So maybe I'll even say a word or two, how we got into this which is...you know, I think the healthcare system is broken. I think when you're healthy, they just don't measure you very often and when they do, they measure very, very little. So you know, go into a doctor's office now and it looks like the doctor's office 40 years ago, they'll bring out the stethoscope, a few things, and measure, you know, 15 things, say, "Oh, you're great, go home."
Yeah, if you think about where the world is today, we can measure so, so much more. And so the genome is one thing, we talked about that with the diabetes. But you can make all kinds of molecular measurements. You can measure, as you say, all your RNA, all your proteins, all your metabolites, all your lipids in your blood, and you can do your metabolites and your lipids and your urine and proteins, and your microbiome, all these things you can measure.
And we don't know for sure what's important and what's not. But we do know we get a much more complete picture when we do that. It's like, looking, you know, at...say you're doing a jigsaw puzzle is what I would say we're doing now. Where if you put out five pieces, that's how medicine is today, you try and guess what that puzzle is like, or what is the picture in the puzzle. You really don't stand a very good chance from 5 pieces if it's a 1,000-piece puzzle. When you put all 1,000 pieces there, you have a pretty good idea what that picture is. And that's how we view health, we want to get the 1,000-piece picture on everybody. And we want to do it over time so we can see if that picture is changing.
So basically, that's what we're doing, we're profiling people very, very deeply, and then we do it over time so we can see the shifts. And one thing we've learned is that everybody's profile is different. I know that sounds obvious, but people don't realize how different they are. And in fact...and it doesn't matter which measurement we use, whether we're following your proteins, or your metabolites, or your lipids, your pattern will be very, very different than mine. And it'll be fairly stable over time, believe it or not, there will be some things that'll change but for the most part, it's the same.
And not only that, what happens is if you get sick, say you get a viral infection or something else, your profile will shift. But believe it or not, you will still look more like you than me when I'm sick. So what that means is that it's very hard to tell the difference when somebody is ill if you're comparing them to everybody else. But it's really easy when you compare them to themselves. So that's why we think these profiles are really important while people are healthy so you can detect that shift really, really easily. And it turns out that that's been very, very important.
So in our study, we have 109 people, and just from the first little over 3 years of profiling, 49, almost half, learned something important about their health. And it was all kinds of different areas. Some was in the area of cancer, some was in the area of cardiovascular, other the metabolic space. And just as some examples, we caught some with early lymphoma. Two people with pre-cancers, they weren't cancers yet, but they have a good chance of turning into cancer. We caught it early, they're called MGUS and smoldering myeloma. And then there were two people with serious heart issues, they had no idea. One was a really young guy, from his genome sequence, we figured it out. And another one is from wearables, and so on and so forth. Caught people with diabetes who didn't even know they had diabetes. And then we saw people become diabetic.
And it was no one technology. That's the power of this, this global profiling let us see the whole picture. And so sometimes it would be, for example, the genome sequence that discovered this, sometimes it might be the protein markers, and sometimes it was imaging, and it was no one, again, technology that did it. Sometimes it's the combination. See, well, the image looked a little off. Look, these protein markers are off. Let's do some follow-up there, and sure enough, you'd see the person had an underlying condition always before symptomatic. So it's very, very powerful. Half of these people learned, again, some pretty darn important things. You don't want to learn about you have a heart condition by getting a heart attack, that's not the way to learn. So we think this big data profiling is very, very important.
Dr. Patrick: Do you think that the trends from, you know, the way the healthcare system is now to this more precision medicine system that you're talking about where it's, like, you're gathering all this data from people and you're making very, you know...you're making decisions based on their personal data and a lot of it. Do you think that's something...like, how do you think we're going to be able to transition to that point because we will get there, right?
Dr. Snyder: Right. So there needs to be a change at so many different levels. One is don't mistake, what we're doing is a research project. But what we've learned is that what kinds of measurements are powerful that, you know, medicine can use. So once again, we've spun off a company. I'm a believer, academics are great at proof of principle and discovering things, but they're terrible at scaling. So we've formed a company, in this case, Q Bio that does a medical version, what I was saying. And it's not cheap, it costs $3,500, which some people can afford, but most people probably can't right now. But I hope, as time goes on, we'll get it cheaper.
We would still argue getting a thorough exam where they do deep molecular measurements and a whole-body MRI is still very powerful because the same thing, we caught a lot of diseases early. Some with early pancreatic cancer, for example, prostate, heart conditions, just from the first bunch of people we've been profiling. So we know this is powerful. Now, why won't medicine do it? Well, first of all, the system is broken, once again, nobody pays to keep you healthy. Medicine in the U.S., people typically get paid when they're ill. So if you know, you walk into a hospital that's when the doctor gets paid. Nobody...if you're healthy, nobody is going to pay you if you walk into a hospital to keep you healthy.
So we need to re-incentivize a system to make it different. And there are ways of doing that I think. So for example, probably pay employers to keep you healthy because then your productivity will be better. So I could see where if we could have, you know, big places, like, Google or Facebook, or what have you have their employees covered by these sorts of things, they would have healthier workers, and that would save them time. I think also economically if we can show...and certain areas, this has been done, like, for cardiovascular disease. You can probably make an argument that it is important to get people measured so they stay healthy because if they have a heart attack and go on long-term disability, that's really expensive.
So I think you have to find these niches. And the other thing you have to do, you have to show...like, insurers don't want to pay unless you've proven to them it works. And this is true for all new technologies even when it's pretty obvious, this is an important thing to do nobody will pay to implement it until you show it works, and it saves them money. Otherwise, there's no reason for doing it. So I think we need to change the mindset of the insurers, we need to have physicians embrace this stuff, that's another thing.
When genome sequencing first came out, we told people we're running around sequencing healthy people's genomes, a lot of physicians freaked out, told me what we're doing was wrong. They still tell me what we're doing is wrong, that we shouldn't be profiling so deeply, because you're going to learn all these things you're going to break the healthcare system, you're going to turn everybody in a hypochondriac. And I think that's just very demeaning to people because I think people...it's just very paternalistic. People are very good at deciding for themselves what they want or don't want in terms of information. And getting this information to catch disease early is a no-brainer to me, and people are going to handle it. Now, actually, they're warming up to the idea of genome sequencing is okay. But I guarantee 10 years ago most physicians thought this is a really bad idea.
Dr. Patrick: Well, you mentioned...and I think that not only are people warming up to it, there's a whole movement of people that are wearing these wearables. They're wearing their FitBits and their Oura rings to track their sleep and, you know, all the other devices that are out there. You know, what do you think is a good start for people that are interested in tracking their own health and understanding, you know, what they can, you know, about themselves through wearing some of these wearables that are available to them? For example, like, heart rate or body temperature fluctuations?
Dr. Snyder: So, great question. So I would say for the big data as a whole, the world has not warmed up to that yet. But you're right, there's a subset of people who are, you know, eager beavers to be quantified, this quantified self-movement. But I think as far as spreading into the general population, you're right, wearables are an area that's starting to have power, but even the medical establishment is still fairly resistant to wearables, I would argue, but they're gaining traction.
They started out as fitness trackers and the way we got involved was when they started out as fitness trackers, Apple Watch didn't exist. We said well, gosh, these are pretty good you know, physiological monitors they're measuring, as you say, heart rate, skin temperature, more limited number of things at that time. Now they measure all kinds of things heart rate, heart rate variability, respiration, even your blood oxygen, even though it's not accurate, it measures your changes pretty good, and blood pressure. Yeah, all kinds of different things you can get from a smartwatch and many of those same things from a ring, the Oura ring, for example.
So they're very, very powerful. And if you think about it, they're measuring you 24/7 and they're taking hundreds of thousands of measurements every day. Some of them will make millions of measurements every day. And so they're really getting a detailed view of your physiology and we think that's super powerful. And so what we discovered early on, we put these on folks, and once again, that's probably the second most important thing I learned from monitoring myself was when I got Lyme disease. I figured out from a smartwatch and something called a pulse ox, it measures your blood oxygen. And the story there, if you'd like to hear it, was I was...you can tell I measure everything. I mean, I'm wearing four smartwatches right now. I normally have a ring, but I lost it. And glucose monitors, the whole shebang.
So anyway, with these smartwatches...or sorry, with the Lyme disease, I was helping my brother put up fences in rural Massachusetts. And then two weeks later, I was flying to Norway through Frankfurt, actually, and on this last flight, I measured myself as you know. I always wear pulse ox because it turns out your blood oxygen drops on airline flights. Most people don't know that, most pilots do, most flight attendants don't. But anyway, your blood oxygen does drop. It's not well documented how much it drops we've now documented all that. But it was pretty clear to me when I flew from Frankfurt to Norway, my blood oxygen dropped abnormally low, it dropped at 90 when it would normally drop on that kind of a plane to 96. And it never came back to normal and I saw my heart rate was running high. And then when...yeah, and same thing, it stayed high. And then I later learned my skin temperature was up too, all measured from my smartwatch.
And then I had no symptoms at that point but a day later, I started getting some mild symptoms and they didn't go away. So I went to a doctor in Norway, I warned him it might be Lyme because of the timing was two weeks. And he drew blood. So my immune cells, called monocytes, were up. He said, "Yep, we've got a bacterial infection." He recommended I take penicillin. I said no, I need doxycycline, which is what you use for Lyme. Was a little tense moment there because, you know, doctors don't like their patients telling them what to do. And he was no exception, that's for sure. He did give in because I was about to go above the Arctic Circle, and I did not want to be sick.
And he gave it, and it cleared up right away, you do take it for two weeks. And when I got back, I got tested. And sure enough, I was Lyme-positive, my antibodies even had some antigen, some proteins from the Lyme that were still there. And it's well-controlled experiment because I had given blood three days before I left. And sure enough, I was negative so I seroconverted during that time. So the key part of that story is actually figured out when I was first getting sick from my smartwatch and a pulse ox and it was how I detected my Lyme before symptoms.
So with that, we realized that these are really powerful devices for measuring when you get ill. And so I had two years of data at that point on my smartwatch. And so we went and looked over all the data. And it turns out I was ill four times during that period. One was the Lyme case, two times were viral infection, and the fourth time I was asymptomatic, but I know I was sick because there's a protein called C-reactive protein that was elevated, and it was just as high as my viral infections and Lyme. So there were four times I was ill. We looked at the data and every single time, my resting heart rate and my skin temperature was up and was up before the symptoms appeared.
So we wrote an algorithm...it works for heart rate, doesn't work for skin temperature. We wrote an algorithm that follows your baseline and looks for a jump in your heart rate, resting heart rate I should emphasize, and it worked. So retrospectively, we could show every single time I got ill my heart rate jumped up early and it was advanced symptoms. It worked on me and it worked on three other people who also were ill and were wearing the same smartwatch. One of them got sick twice. Every single time, we could see the jump up in heart rate before symptoms. So that really showed that these are incredible health monitors. And these weren't expensive devices, these were like...especially at that time, I think it was something like a $150 watch that was doing all this. And I know you can do it for a $100 watch.
So as you might imagine that when COVID came along, we had been building out improving our algorithms, building an infrastructure to do this at scale. I'll come back to what that means in a minute. But what we can do now is...and when COVID came along, we quickly enrolled, opened up the study partner with Fitbit, Garmin, and launched a study to try and first show if we could detect COVID with a smartwatch. And then the second part, which we're in now, is alerting people if their heart rate goes up.
And so what we're doing for the first part, we showed that with a smartwatch, we can see people's resting heart rate jump up. We had 32 people wearing a Fitbit. At the same time, they had COVID and they had a diagnosis date and a symptom date. And we showed that for 26 of the 32, we could detect the jump up in resting heart rate, and in basically in nearly all cases it was at or before symptoms. So 81% of the time, we can see people's resting heart rate jump up with COVID. And then we have now...and it turns out, by the way, the very first case we had, it was 10 days early. Somebody...is a very clear signal, you can see this person's heart rate jumped up 10 days early. On average, it's about four days. So people's heart rate will jump up four days before their symptoms if they have COVID, it turns out, and that we can pick up with a smartwatch.
So we're now...we've written some algorithms to do this in real-time, comes back to what I was telling you before, so you follow your baseline and you look for this elevation in resting heart rate. We have three different algorithms to do this. And so we'll profile you...I don't know if you've signed up for this study yet, Rhonda, I hope you have. So anyway, it builds an hour-by-hour measurement of you. And when you jump up, you know, pretty high for extended periods, say 6...these days to keep the false positive, it's more like 12 or 24 hours. If you're up for a while and it's statistically, you know, unlikely, it's not a random fluctuation, it's up there, we send an alert. And it turns out it works pretty well. So 70% of the time, we can detect illness.
We had 63 people as of the end of January who had COVID, and 44 of them, we could detect in real-time and alert them before or at the time of symptoms. So it's not perfect, it needs a lot of tuning still, that's why we want people to enroll in our study, we want to basically improve the algorithms. And we don't...it's not just specific for COVID -- other illnesses will trigger it. And also other things will trigger it, like too much alcohol, not a drink or two, but if you really tie one on, you know, it will send your heart rate up. Hiking in the mountains will do it too. So you have to contextualize it. But it does work in general for detecting respiratory illnesses. And so with improvement in algorithms, I want to be able to tell the difference between, you know, drinking too much versus the respiratory viral infection. I don't yet know if we'll tell the difference between flu and COVID, we'll have to see.
Dr. Patrick: Where can people go to sign up for this COVID tracking study with their wearables?
Dr. Snyder: Yeah, go to innovations.stanford.edu/wearables. So innovations.stanford.edu/wearables. And we'd love to have you enroll, and it does work. I can show you a picture, you'll see, you'll get these red alerts. And then we want you to respond and say, "Yeah, here's what I was doing," if that happens.
Dr. Patrick: We'll put that URL in the show notes as well. So I, kind of, want to shift back and ask you about heart rate variability, you mentioned that. What can people learn from their heart rate variability data that they're getting from their whatever, fill in the blank, wearable they're wearing?
Dr. Snyder: Yeah, great question. So heart rate variability...this might sound a little funny to you, but you're actually supposed to have a variable heart rate. If it's totally constant, there's something wrong with you, actually. So it's a measure of health, so it should it be shifting around a little bit. And yeah, I mean, it's one of these parameters it's a sign of your health. And there's other measurements too like when things go up with some of these measurements, you can actually pick up atrial fibrillation basically, afib, as it's called, can get picked up by your smartwatch. Right now there's a high false-positive rate but some people have picked that up from their smartwatch. You can even get an electrocardiogram measurement from an Apple Watch, you may know, and some other devices now.
So those you can measure and they give you some information. Again, there's still some noise that people are working through and that's why we need to tune the algorithms better and get more data. We ourselves are very focused on the infectious disease detection, other groups are more focused on heart health. But heart rate variability is a key measure of heart health if you will.
Dr. Patrick: So to, kind of, shift gears for a minute and talk a little bit about some of your other data, which I found really interesting, this had to do with the exposome. Am I saying that correctly?
Dr. Snyder: Yeah, exposome.
Dr. Patrick: Exposome. I'm not sure people know what that is so maybe you could, kind of, start there just explaining what that is for people that don't know.
Dr. Snyder: Yeah, your exposome is all the things you're exposed to. And what we're measuring is your airborne exposure. So we have a device, this is the second generation, a third one's coming that's smaller. What it's doing is it's sucking up air at about one-fifth of what you breathe. And what we have, it's measuring things like PM 2.5, and temperature and humidity. But the power of this is that it actually has a filter under the intake valve that captures all the particulates like pollen and bacteria and fungi that you're actually breathing. And under that, we have a chemical absorbent that sucks up all the chemicals that you would also be breathing.
And then we analyze them, we don't analyze them in real-time, we take it apart and take the cartridge out actually. And we can measure all the biologicals, meaning pollen, and bacteria, and fungi that you're exposed to. And we can measure all the chemicals that you're exposed to too. You know, pesticides, turns out there are plastics everywhere, pesticides are everywhere, but their amounts will vary quite a bit. And certain carcinogens are everywhere, too. And some locations will have a ton of this stuff and others, you know, generally not so much. So that's what we're trying to measure.
And the ultimate goal is to try and understand how exposures will contribute to, you know, your disease. Because there's no question that your risk for disease, it depends upon genetics, but it also depends upon environment. And we think this is...that's the one thing that's always been very poorly measured is the environmental exposure. So that's what we're actively working on now, amongst other things, to try and capture that information.
Dr. Patrick: It's also the one thing that's not as easy to control. For example, you know, you can make a decision about what you're going to have for breakfast, lunch, or dinner, or whether you're going to fast and not eat or, you know, when you'll eat your food or if you're going to exercise. But the things you're breathing in, with the exception of, I guess, if you live somewhere close to a, you know, busier street or a highway, for example, where there's likely to be more particulate matter and air pollution and benzene, it's very difficult to control the air you're breathing in.
And there's been so many studies that have been coming out over the last few years. And of course, these are observational studies. There's all sorts of potential confounding factors that come along with observational data. But I think, you know, there has just been a pretty, I think, clear picture that air pollution increases the risk for a variety of age-related diseases in addition to just, you know, respiratory disease, Alzheimer's disease, you know, for one.
I mean, this is even something that's been shown in children that live in, for example, Mexico City, that have, you know, passed away. There's been some post-mortem studies that have looked at amyloid plaques in their brain, and it's just, like, looks like an old person's brain in a young child in a place where the air pollution and air quality is so poor. So have you guys been looking at, you know, maybe where people are living or if they have a HEPA filter, or some kind of filter, whether or not that makes a difference?
Dr. Snyder: So, great question. So the answer is...I'll say to some extent, what you're talking about is the more non-specific stuff like pollution, smoking, we know those are harmful, no question. And so we have looked at that, we actually discovered it looks like for one group we were studying speculated that actually there's some heavy metal mining upstream, and they speculated there's a high incidence of autoimmune disease. They thought that that might be due to the mining. And actually, it does correlate that way that as people live along the river, we discovered actually are seen to have a much higher incidence of autoimmune disease. So I suspect their hypothesis is correct. And so smoking, yes. I mean, those are documented studies by a lot of people, you know, inner-city kids, you know, exposed to pollution have a lot of this. I'll back up a little bit though. I do think you can have a better control, at least some control over this, in the sense you mentioned HEPA filters, sure, that's good.
But one of the things I discovered...I would argue we don't really know enough to make informed decisions about what's going on. And as a good example, I used to have more severe allergies, they are, kind of, mild now. And I always assumed they were pine, they came out, you know, April, May, like everybody's. But then when I actually did the correlation, when I looked at my data, and I looked at allergies, something called eosinophils, which are involved in your allergic response, and I correlate it with my exposures and guess what? Didn't correlate with pine, it correlated with eucalyptus. You say, well, how's that actionable? Well, I got two trees behind my house, a pine and eucalyptus. If I'm ever going to take one of them down, you can guess which one goes down first, it's going to be that eucalyptus tree.
So I honestly think that having more information can sometimes lead to more informed decisions. And I hope that'll be true about some of the other technical things. Like, there's just a ton we don't know. It's been speculated, you know, why are, you know, girls reaching puberty earlier? And it's been speculated that some of the plastics look similar to, you know, estrogen, and nobody knows if that's true or not. How do you know? There's never been a proper study to do that sort of thing. We can make those measurements, we might be able to see if any of that's true. And so I feel like we need...everybody knows the environment, you know, is important for disease, but we don't know what aspects of the environment. Crohn's, you name the disease, Crohn's, you mentioned aging, absolutely true. It's there and it's just never been measured.
So we don't know exactly which molecules are leading to these problems. Some of them may be just general particulates, like pollution, air pollution, but some of it may be very, very specific ones. And let's see if we can get those things outlawed, like, right get those metals out of the gas, was something that was...and now the paint was something...get lead out of paints was only because studies took a while to realize that lead was causing, you know, neurological problems. And so you have to identify that, you have to measure it, you have to see it first to know what's going on. And I think that's what the measurement is all about, you know, we're just taking tons of measurements. You're exposed to thousands of species, and which ones are associated with what aspects of your health? We don't know until we measure it.
Dr. Patrick: Have you guys measured...done the exposome of firefighters, people that are, you know, fighting these wildfires?
Dr. Snyder: Yeah, believe it or not, we are. So when these fires in California burst out, we've been trying to get our monitors out to as many people as possible. And including firefighters, you have to put them a little carefully because they obviously can't interfere with their duties. But yeah, so we are trying to do this. And I don't know what you know, but it's something you alluded to that kids in these poor areas, like in Fresno where there's a lot of pollution, where there's a lot of firefighters, there's a lot of studies that show that they have a much, much higher incidence of allergies and asthma when they're in these areas. And it does seem to be associated with firefighters.
So we're trying to measure exactly what they're getting exposed to. And maybe there's some way to help control that or figure out ways to try and extract that, I guess we can see what the harmful elements are. Maybe even if we can't control the exposure, we'll try to as much as possible to expose, but maybe there's a way to try and chelate it and remove it out of focus. I don't know, that's not exactly my area of expertise.
Dr. Patrick: I do know a little bit about not chelating but...so there's a couple of...not to get too far off-topic, but you might find it interesting. So one, there's a compound found in some cruciferous vegetables, particularly in broccoli sprouts, the young sprout of mature broccoli, called sulforaphane, which has been shown in now quite a few studies. There's been, you know, intervention trials where people are specifically given sulforaphane concentrate, and it causes...so a lot of these studies have been done in China where there's also terrible air pollution problems. It increases the excretion of benzene, which is found in you know, air pollution, cigarette smoke, for example, by, like, 60% after 24 hours. Also acrolein is now the one that it increases the excretion of...by activating the Nrf2 pathway, which then downstream a lot of these phase two detoxification enzymes get activated, for example.
The other interesting thing is sweat. And you know, there's been a variety of studies that have looked at which kind of, for example, heavy metals or other xenobiotic, like, parabens or BPA, things like that, which are excreted through a variety of different, you know, mechanisms. Some are excreted more prominently through urine and others through sweat. And so things like exercise and even sauna bathing can...you know, for example, mercury is one that really is excluded through sweat. So you might find that interesting.
Dr. Snyder: Yeah, I've heard a little bit but you've told me a lot of new stuff I absolutely didn't know. So great, thanks for sharing that. No, I think detoxing for mercury is definitely something that's been out there for a while. Of course, I grew up with that stuff.
Dr. Patrick: Yeah, everybody had the mercury amalgams in their teeth.
Dr. Snyder: Yeah, we used to play with that stuff when we were kids when the thermometer broke, we used to stick our hands in that, that wasn't such a good thing to do.
Dr. Patrick: So I wanted to talk a little bit about the ageotypes, and how you've used all this data, you know, a variety of, you know, metabolites, and the proteome, and the genome, and just other biomarkers as well, to, kind of, look at how people are aging. And what their predisposition is to, you know, a disease of the brain versus a disease of the heart versus a disease of the liver, for example.
Dr. Snyder: Well, I mentioned before that we take tons of measurements on people including their microbiome and all kinds of molecules. And for the most part, your molecules don't change. There are interesting time...believe it or not, there are seasonal changes. And we argue there's two seasons in California. So you'll see changes in some molecules with seasons. But the other is by following people over time, we can see how they're aging. And it's the first time it's been done in this kind of detail. And so normally, when they study aging, they look at difference between old people and young people and say, oh, old people have this and young people have that.
And therefore, like, hemoglobin A1C, marker of diabetes, old people have, you know, more and young people don't, therefore, it changes over time. And what we discovered...and I don't think it's a surprise, but it's nice to show is that people are aging differently. So I'm a metabolic kidney, liver ager, but my immune system is not aging so much. Another person, he's a cardio ager, his cardiac pathways are changing the most rapidly over time. We think you only need about five measurements within two years, we can tell how you're aging, and again, everybody is aging differently. So we think of it, like, a car where, you know, you have a car, the whole thing does get older, but some parts wear out first. And so we think that's what's going on.
And you know, the cardio ager, the heart, we later learned that person was stage two hypertensive, which kind of fits with the idea that cardiovascular system was going off. And so in the end, we had 43 people with enough data, we can group them into these classifications, ageotypes, we like to call them, what's your ageotype? And it was kidney, and liver, immune, and metabolic aging. Now, I know there's more than that, there's a cardio ager, but we only had one of those, so we didn't have...there'll be many categories of ageotypes. And we're about to analyze more people soon so we'll see just how many categories we can come up with.
But everybody ages differently. And so you might say, so what? And by the way, we can see some people will go up...there's clinical markers associated with these. And the metabolic ageotype, you'll see people's hemoglobin A1C and other things going up. But what's kind of cool is some people have theirs going down. So what did they do to make theirs go down? Well, you can go back and look at the data and some people did, exercise is an easy one. They exercised, they lost weight, and that makes a lot of sense.
But there's other things we didn't realize, like, there's a molecule called creatine which is a marker of kidney function, and we discovered that's known to go up over time. But we discovered we had a whole bunch of individuals who were going down for the creatinines, like, what's going on there? Well, 8 out of 10 of them were on statins. So our hypothesis is that the statins might be helping. It could relate to muscle mass, but we didn't detect any changes in muscle mass based on some of the measurements we're doing. So it may be that statins improve kidney function, nobody really realized it, that's possible. It's something we're going to follow up on.
So by correlating, you know, how people are changing, we can see what's going on. I think we can do more than that. I think if you're a kidney ager, maybe you drink more water. If you're a liver ager, maybe you shouldn't drink so much alcohol. You know, we think, again, it's actionable information. If you're an immuno-ager, maybe you want to take, you know, turmeric or curcumin. Some garlic things that should, you know, help with your immune system, give you a little immune burst. So we think the information does have value and now we can run trials on the stuff.
Here's another interesting way to look at it. In today's world, if you walk into a drugstore, you'll see a whole aisle on supplements, you know, a lot of them purporting to, you know, give you longevity. And you'd have no way of knowing if that's working. Almost anything that's put out there that tells, you know, this works for increasing your lifespan, how do you know? There's no way of measuring. So we think by measuring these people's ageotypes, if you will, it's in a timeframe that's actionable, you can see how people are aging, you try an intervention and see if you can reverse it or at least slow it down.
Dr. Patrick: Was there any biomarker, or biomarkers plural, that correlated with, you know, just aging in general? So like, let's say your hbA1c was really good as you were getting older. But that wasn't necessarily going to tell you whether or not your immune system was still aging, or your liver. You know, was there something that was a little more universal like an inflammatory marker? Was there something that, kind of, could maybe affect all these organs?
Dr. Snyder: Well, yeah, you're getting in an issue that's of high interest to the longevity field, the aging field, is you know, are there some, you know, panaceas that can actually slow down all these things? And most people if they want to find the systems-level control of aging, they're trying to do it through metabolic health. And so people like the idea of this drug metformin, it might be a way to systematically slow aging. And there are trials now running for that out there to see the metformin. It's been a widely used drug, it comes out...the first observation was that diabetics on metformin seemed to live a little bit longer than normal people. They never did the right control showing normal people with metformin would maybe live even longer, too. So that's what's, kind of, going on now.
And so there is interest in that. I don't know what to say about that. I think it is worth trying. I think there probably are some general metabolic control. A lot of people like the idea that your unfolded proteins are going off so if you can do things that might promote, you know, better proteostasis, if you will, you can actually get people to live longer. There's a lot of interesting things out there so we'll have to see. It's a very active area. A lot of people are now starting to invest in this. So it went from being almost a bizarre phenomenological field to...still is a bit phenomenological. But people are really trying to do active treatments to control aging, I guess, in part because we have an aging population, and people want to do something about it.
Dr. Patrick: Yeah, just, kind of, speak to metformin, you know, that field and that sort of arena of people that think that might improve longevity. I was, sort of, very interested in it as well. That study that you mentioned was probably the major thing that caught my attention. But then there's been a couple of randomized controlled trials that have come out since then showing that healthy...so people that don't have type 2 diabetes. Healthy people that are physically active, doing resistance training, and/or even aerobic exercise, when they take metformin, it blunts some of the benefits, exercise-induced benefits that are improving a variety of things. So that was really discouraging for me, at least, in terms...like what you'd want to see as it synergize or, you know, or it has an additive effect or something.
Dr. Snyder: Absolutely.
Dr. Snyder: I saw the same study and had the same reaction, yeah. And, like you, I exercise every day so it's very disappointing to see that because it abrogates the effects of exercise, metformin does.
Dr. Patrick: And I think, wasn't there a study that compared exercise to metformin use and found exercise was actually better at...I don't remember what their marker was, if it was insulin sensitivity, if it was some other marker of glucose regulation, I don't know what it was. But that exercise was actually better, I think, I remember reading.
Dr. Snyder: Well I didn't see that. But I can imagine that to be the case. Exercise induces a lot of stuff that's beneficial, myostatins, all kinds of useful things, endorphins. And the other thing, especially for aging, in fact, if you talk to anyone in the aging field, almost all of them will say exercise is number one for longevity, food, number two. And you know, I can see why they would say that. When people get older, you know, one of the number one problems they have is sarcopenia. So you know, loss of muscle mass and exercise certainly keeps that up. And now there are studies...they used to tell people who are 80, you know, old take it easy, relax so you don't hurt yourself. But actually what you really want them to do is just the opposite. You want them to get up out of the chair and move around because they'll actually live longer and be healthier than if they just sit around in their chair. And now there's studies out there like that.
So, exercise, there's no question it's very beneficial. We don't even understand how it works. It's pretty cool, there's a study ran by NIH that's launching now, or launched a few years ago but we're in the middle of it. It's a $170 million study to try and understand the benefits of exercise both aerobic training, so running, biking versus resistance training, and see what promotes, what benefits, and how does it work. It'll be very fun to see what comes out of that study.
Dr. Patrick: Totally. And you had a study that was published not long ago on some of the metabolic changes of exercise.
Dr. Snyder: We did, yeah. So we did the same deep molecular measurements on people who did exercise. We discovered half your molecules change when you run to what's called your VO₂ max. Your VO₂ max is also an indicator of longevity, it's actually one of the best indicators of longevity. So we did, we saw changes we could see that, you know, a lot of immune molecules shifted. And that makes sense, you boost your...you know, you remodel your muscle mass, to be honest, when you exercise, especially with resistance training. And then all kinds of metabolic control markers changed too.
And I'm sure all that stuff's very, very powerful in the context of the current pandemic, the COVID-19. Being able to have, you know, a strong immune system is really key, I think, to longevity. You may not know but you're getting cancer your entire life, and you're clearing it your entire life. Why is it that old people get cancer? Well, what happens is your immune system declines, especially in people in their 60s. And so suddenly, these cancer cells that you've been clearing are getting old, and then they can actually burst out and you get cancer. So I think keeping immune health is, in my mind, probably the number one thing and exercise definitely promotes immune health. All kinds of beneficial cytokines and other factors are induced by exercise. So yeah, I think it's...
Dr. Patrick: Do you think that there's a bigger component for genetics or lifestyle in some of that, like, how your immune system is aging versus your heart or your liver? Is it a combination of them or is it one or the other?
Dr. Snyder: For sure, it's a combination, yeah. How much of aging is due to genetics, there's no question there's a strong genetic component. You look at centenarians, they run in families. But there's also a strong environmental component, you don't have to look past smoking, or some of the things you described earlier, living near highways, to see how to, you know, decrease people's lifespans. And so a lot of risk factors of all sorts have been associated with lifespan. So the one thing about the environmental factors, the hope is that we can control that, and lifestyle factors. Those are things we do have control over, genetics is a lot tougher.
Dr. Patrick: Well, being mindful of your time I, kind of, just wanted to wrap up. Maybe, you know, since you are monitoring all these things, and not only studying other people but yourself, maybe kind of...it'd be interesting to hear your lifestyle routine, like your exercise routine, maybe like your meals or you know, like a sample of what your general meals are, how much...if you do fasting... time-restricted eating?
Dr. Snyder: So I do exercise every day as you can probably tell. In fact, I do weight training, You can't tell but I actually gained 10 pounds of muscle mass since I started this. I do whole-body MRI too, from Q Bio. So I do exercise every day, even though it didn't help me with my glucose control. That's how I started, I thought muscle mass would be better for glucose homeostasis, that failed on me. But I still do it anyway because quite frankly, it makes me feel good and all those other benefits we talked about earlier, sarcopenia.
And then yeah, because I am type 2 diabetic I try and avoid carbs, I tend to eat a lot of protein. So you know, eggs and protein-rich foods. One problem with me is that I don't like vegetables, and that's a terrible thing. It's something I've never gotten over all kids have that. So I eat a lot of salads and things. I do like carrots and that sort of stuff. So I am trying to make up for it. You may know that most people are very fiber-poor, meaning what you're supposed to get...depends on whether you're a woman or a man, but you're supposed to get about 30 grams of fiber a day and most people get about 12, sometimes 15. So I'm trying to be conscious about eating more fiber as well from carrots and things like that. But I will be doing fiber supplementation as well to try and get those numbers up. And I eat a lot of nuts, they have omega 3s, things like that.
So, I guess that's my lifestyle. And I don't meditate. I was meditating, that probably is good, that's supposed to be good for, you know, your synaptic neurons and things. So yeah, I need to get back to that, that's something I just haven't found time for but should.
Dr. Patrick: Yeah, me too. I always...if it's between exercise and meditation, I always go for the exercise because I feel like I'm getting...I can get a meditative state from that as well. But just real quick on your lack of vegetables. I'm interested in your microbiome data, is that something...have you experimented with how your personal microbiome looks, you know, versus if you're eating more vegetables, or not?
Dr. Snyder: A little bit, your microbiome, believe it or not, doesn't shift that much, you really have to make a long-term commitment to shift. If you take an antibiotic, you'll shift it, and then it bounces right back, believe it or not, as soon as you go off the antibiotic. Now, some of your strains will change but the general composition is pretty similar if you take an antibiotic. But some of the sub-strains...which may be important, some people are still trying to figure that out.
For me, I can tell one thing that works, Lactobacillus reuteri, you know, maybe a little gross, but gives you the stool composition you're looking for. I did try that and sure enough, it does work. These days with my fiber diets and various things I eat, I haven't worried about it because I do seem to be pretty well set up that way. But I have done that. And I'm about to try some other experiments. I've been doing all kinds of...our lab is doing all kinds of fiber experiments to see what fibers do what to what microbes, and we have seen some very interesting shifts.
You hear fiber is good for you but you may not realize but there's all kinds of fibers out there. There are what are called long chain and short chain, and hydrophobic, meaning greasy, and hydrophilic meaning water, you know, loving, and you know, positive, negative. It's like saying all animals are the same, they're just all different. And so we're trying to see which fibers do what. So we have some academic studies going on there. Yeah, we have a good one that is known already but the literature is very, very confused on these. But this one is very, very clear, which is arabinoxylan which is found in psyllium husk will actually drop your cholesterol. That one is pretty clear.
Dr. Patrick: Oh, that's cool. So there is a...like you mentioned earlier, the associations between microbiome composition and metabolic health, like type 2 diabetes, for example. And there's also autoimmune connections, if I remember correctly, as well.
Dr. Snyder: There are yeah, there is a lot of connections between your microbiome. And our case, by the way, we know microbes correlate with that drop in cholesterol. So we think they're an important part of that and, in fact, it's the way they're dealing with the bile acids, we think they suck out your cholesterol.
Dr. Patrick: Oh, really?
Dr. Snyder: Yeah, it's a very different mechanism that people appreciate that we've learned by doing the steep profiling. And so we do the...
Dr. Patrick: What's the strain again?
Dr. Snyder: I don't remember the exact strains that were doing it but they were microbes that seem to be elevated. And what we think they're doing is they're actually making more secondary bile acids, which bind cholesterol and actually remove it from your blood. And that's how we think it lowers, that's our model, we haven't proven that. That's how we think you can lower your cholesterol with this fiber. Which I don't think anybody appreciated before because they hadn't seen all these different components.
Dr. Patrick: Have you heard about people...there's a lot of anecdotes out there and might even be published data about L. reuteri actually lowering cholesterol as well.
Dr. Snyder: Yeah, that didn't do it for me, but that could be a personal thing, it's possible. Lactobacillus in general, you know, the bifidobacter and lactobacillus, those are your beneficial microbes, as you probably know. And so in general, things...and fibers generally increase both of those. So that's one way in which they promote this. They're thought to actually make something called short-chain fatty acids, which give your immune system a boost. So that's one way in which fibers are thought to do it.
But it probably is the case that different people react to different fiber, it's very clear they do. And that depends on your microbiome because your microbiome will degrade the fibers differently. And so the microbes you have will degrade a certain set of fibers that's different from the microbes I have in my gut. And so that's one of the reasons we are different in our metabolic health.
Dr. Patrick: Do you think there's a good reason to measure your personal, you know, microbiome, like, for example, in your fecal...there's quite a few companies now, you know, that are available to consumers, you know, where people can give a little sample and see what's in their gut basically?
Dr. Snyder: Right, right. So the answer is yes. Microbiome, it's one of these things everybody knows is super, super important. But the actual showing something with clinical value has been really, really tough. So, a lot of companies have formed, and a lot have gone away. And we know that there is something there and it's a matter of getting the right understanding, I think, to go with this. Because I think, ultimately, knowing your microbiome is really going to be important for knowing what foods you should be eating.
And so some of the companies that are forming around this area, there is going to be value in all that but it's not all worked out yet, but stay tuned, I think it's coming very, very soon, actually, and how it relates to immune health and such. So it's, kind of, interesting because you may not know, but you have more immune cells in your gut than anywhere else in your body. And it's because they're actually in this interplay with your microbiome that's in your colon, in your feces.
So basically, there's this interplay between your immune system, your microbiome, and the food you eat, and it's a three-way access. And so as a direct link, if you will, between food, what's going on in your gut, and your immune health. And then obviously, your metabolic health since your microbiome is making all these metabolites that show up in your bloodstream and are critical for your whole metabolism. So, it's a whole interplay.
To us, this is why the big data is so important, because it gives you a better understanding of your whole health picture not, you know, just some 5 or 10 little analytes that it gives you, again, just a very, very narrow view of your health. So this is why we think these big picture...and ultimately food logging is a pain, you probably have done it. We need better ways to food log because I think that will help. And they're coming, they're better than they used to be. But I think that's going to be critical knowing your food health, again, and your microbiome and all these things. So you can put all the pieces together, and really make healthy people without having to take drugs, quite frankly. I wish I didn't have to take any drugs, but I have high cholesterol and I have high glucose so I'm taking two, which I'd prefer not to if I can control other ways.
Dr. Patrick: Well, Mike, I am so excited about the research you guys have been doing and are continuing to do. I think that this big data approach of just measuring as much as you can, I think you're going to find unique associations in biomarkers and, you know, not just looking at the microbiome, but looking at the microbiome and the metabolome and the genome and the proteome, and looking at the whole picture. It's a very exciting time so I look forward to continue to follow your work.
Dr. Snyder: Thanks.
Dr. Patrick: For people that want to find out more about what you're doing and also just follow you in general, so you are on social media, you're on Twitter.
Dr. Snyder: Yeah. SnyderShot is my Twitter feed, so to speak. And then, yeah, if you want to sign up for any of our studies, there's innovations.stanford.edu/wearables for the COVID one, or just go to innovations.stanford.edu and you'll see we have other studies going there as well. And then we have spun off, like, the continuous glucose monitoring, January AI is a company that's trying to improve metabolic health using that kind of technology. And Q Bio is doing the deep data profiling on people, again, trying to get a very complete picture. It's much more medically relevant, as I say, than the research one we're doing in the lab, but both are a lot of fun.
Dr. Patrick: Very cool. Well, thank you so much, Mike, and it was really great having you on the show.
Dr. Snyder: Thanks for having me.
Hard, insoluble clumps of amyloid-beta protein. Amyloid plaques are a pathological hallmark of Alzheimer's disease. Formation of amyloid plaques occurs well before symptoms of Alzheimer's disease manifest.
A class of bioactive compounds present in many fruits and vegetables. Coumarins exert antioxidant, analgesic, anti-inflammatory, anti-clotting, and anti-cancer properties. The chemical structure of coumarins is similar to that of warfarin, a drug used to prevent blood clots in humans.
A naturally occurring amino acid present in the muscles and brains of humans and other animals. Creatine plays central roles in skeletal muscle metabolism. It is widely used as an ergogenic aid (as creatine monohydrate) to promote performance in endurance and resistance exercise.
A type of white blood cell. Eosinophils initiate and propagate inflammatory responses and modulate both innate and adaptive immunity. High eosinophil levels typically indicate the presence of infection or inflammation.
The totality of non-genetic exposures a person experiences during a lifetime. The exposome comprises both tangible and intangible exposures, ranging from food, air, physical surroundings, microbes, and chemicals to psychological stressors, education level, and financial status, among others, and likely has myriad effects on human health. Assessing and quantifying the exposome presents challenges, but the length of telomeres, distinct structures comprised of short, repetitive sequences of DNA located on the ends of chromosomes, may provide a suitable proxy for its assessment.
A wearable fitness, activity, and health tracker.
The collective set of genetic instructions for a single organism. The genome is stored in an organism's DNA and provides all the information required for its function and survival.
The physiological phenomenon of variation in the time interval between heartbeats. It is measured by the variation in the beat-to-beat interval. Decreased parasympathetic nervous system activity or increased sympathetic activity will result in reduced HRV. Reduced HRV has been shown to be a predictor of mortality after myocardial infarction, and a range of other outcomes/conditions may also be associated.[1]
A blood test that measures the amount of glycated hemoglobin in a person’s red blood cells. The hemoglobin A1c test is often used to assess long-term blood glucose control in people with diabetes. Glycation is a chemical process in which a sugar molecule bonds to a lipid or protein molecule, such as hemoglobin. As the average amount of plasma glucose increases, the fraction of glycated hemoglobin increases in a predictable way. In diabetes mellitus, higher amounts of glycated hemoglobin, indicating poorer control of blood glucose levels, have been associated with cardiovascular disease, nephropathy, neuropathy, and retinopathy. Also known as HbA1c.
A measure of how sensitive the body's tissues are to the effects of insulin. Insulin sensitivity defines a relationship between insulin production and glucose uptake. Poor insulin sensitivity promotes increased pancreatic insulin production, which can lead to increased risk for high blood pressure, heart disease and heart failure, obesity, osteoporosis, and even cancer.
A genus of lactic acid-producing bacteria. Lactobacilli are the most abundant probiotic bacteria found in fermented foods such as yogurt, cheese, kefir, pickles and others. They are also present in the oral cavity, gut, and vaginas of humans and animals where they exert health-promoting properties.
A species of lactic acid-producing bacteria. In humans, L. reuteri is found in/on the gut, urinary tract, skin, and breast milk. L. reuteri exerts antimicrobial properties that inhibit the colonization of pathogenic microbes; benefits host immunity by reducing the production of pro-inflammatory cytokines; promotes regulatory T cell development and function; and reduces the risk of microbial translocation from the gut to peripheral tissues. Consumption of prebiotics that support L. reuteri populations or direct supplementation may reduce the risk of inflammatory diseases.
An umbrella term for cancers that originate in lymphocytes (a type of white blood cell). The two most common forms of the disease are Hodgkin lymphoma and non-Hodgkin lymphoma. Although lymphoma is rare, it is the most common type of blood cancer.
The collection of metabolites produced in an organism, cell, biological fluid, or tissue during metabolism. Metabolomics, an emerging field of study involving the identification and quantification of the metabolome at a specific time point, creates a metabolic profile that provides information about the body's physiological state.
An abnormal condition in which the bone marrow produces low levels of monoclonal protein (also called M protein). Approximately 20 percent of people with MGUS develop myeloma, a cancer of the blood.
A wearable sleep tracker.
A broad class of synthetic compounds used as preservatives in cosmetics, personal hygiene products, foods, and pharmaceuticals. Parabens can enter the systemic circulation via oral intake or via the skin. Evidence suggests parabens exert estrogenic effects in mammals and may influence carcinogenesis, infertility, spermatogenesis, adipogenesis, and mental health.
A mixture of solid particles and liquid droplets. It is present in fine inhalable particles, with diameters that are generally 2.5 micrograms or less. Exposure to air pollution promotes oxidative stress and increases the risk of developing many chronic diseases, including cardiovascular disease, cancer, hypertension, and diabetes. Evidence indicates that global air pollution shortens people’s lives on a scale greater than warfare, other forms of violence, parasitic infection, and more.
Fine inhalable particulate matter (PM) in air pollution, with diameters that are 2.5 micrograms or less.
A portmanteau of the words protein and homeostasis. Proteostasis is maintained through the competing and integrated biological pathways within cells that control the biogenesis, folding, trafficking and degradation of proteins present within and outside the cell. Proteostasis deteriorates with age. As a result, the prevalence of age-related protein misfolding diseases, such as Alzheimer’s disease and Parkinson’s disease, increases.
A non-invasive device for measuring oxygen saturation levels in blood, typically worn on the fingertip while measuring.
A medication used to treat type 2 diabetes. Repaglinide lowers blood glucose levels by stimulating pancreatic insulin release.
An intermediate disease state between MGUS and active myeloma. People who smoldering multiple myeloma have high levels of monoclonal protein (also called M protein) and more abnormal plasma cells in the bone marrow than patients with MGUS. (See definition for MGUS.)
An autoimmune metabolic disorder in which the pancreas produces little to no insulin. Type 1 diabetes is caused by autoreactive T-cells that recognize pancreatic antigens and subsequently destroy insulin-producing beta-cells.
Electronic devices that patients or consumers can wear to monitor their health, fitness, activity, or sleep. Wearable devices can transmit information to a physician or to the user in real time, allowing the wearer to actively participate in monitoring and maintaining their own health.
Member only extras:
Learn more about the advantages of a premium membership by clicking below.
Hear new content from Rhonda on The Aliquot, our member's only podcast

Listen in on our regularly curated interview segments called "Aliquots" released every week on our premium podcast The Aliquot. Aliquots come in two flavors: features and mashups.
- Hours of deep dive on topics like fasting, sauna, child development surfaced from our enormous collection of members-only Q&A episodes.
- Important conversational highlights from our interviews with extra commentary and value. Short but salient.
Metabolism News
- Vitamin D increases muscle strength and mass without altering body weight in mice.
- Mouse study suggests that interleukin-6 (IL-6) may regulate body weight by increasing substances in the brain that trigger weight loss. (2012)
- Metabolism changes not chiefly responsible for middle-age weight gain: result of other (not fully understood) physiological changes, lost muscle
- Acid Suspends the Circadian Clock in Hypoxia through Inhibition of mTOR. - PubMed - NCBI
- Pharmacological activation of circadian rhythm reduced the growth of glioblastoma in mice as effective as standard chemo but w/o side effects.